Review Article: Journal of Drug and Alcohol Research (2025) Volume 14, Issue 1
Spinal Cord Compression by Hydatic Cyst: Case Report, Drug Therapy and Comprehensive Review
Lourdes de Fatima Ibanez Valdes1 and Humberto Foyaca Sibat2*2Department of Neurology, Nelson Mandela Academic Hospital, Walter Sisulu University, South Africa
Humberto Foyaca Sibat, Department of Neurology, Nelson Mandela Academic Hospital, Walter Sisulu University, South Africa,
Received: 20-Dec-2024, Manuscript No. JDAR-25-162721 ; Editor assigned: 25-Dec-2024, Pre QC No. JDAR-25-162721 ; Reviewed: 08-Jan-2025, QC No. JDAR-25-162721 ; Revised: 13-Mar-2025, Manuscript No. JDAR-25-162721 ; Published: 10-Apr-2025, DOI: 10.4303/JDAR/236429
Abstract
We report a 27-year-old lady with a 3-year history of signs and symptoms of progressive spastic paraparesis due to hydatid cyst at the level of T5. We comprehensively searched the most essential electronic databases following the PRISMA methodology and we found five similar reported cases responding dramatically well to the drug therapy with antiparasitic medication after the surgical approach without recurrence.
Keywords
Antiparasitic; Surgical Approach; Electronic Databases
Abbrevations
ELISA: Enzyme Linked Immunosorbent Assay; ELTB: Enzyme Linked Immunotransfer Blot; MRI: Magnetic Resonance Imaging
Introduction
The larvae of Echinococcus granulosus cestode are the causal agent of hydatid cyst, which is a parasitic disease affecting mainly the liver in 60%-70% of infected patients and around 15%-20% have this parasitic lung disease, while only 0.5%-2% have bone tissue involvement; despite this parasitic infection can infest all tissues and organ. This infection is more prevalent in places where livestock and agriculture are common. Fortunately, cord infection is quite rare and has a poor outcome. However, its mortality rate is not high, being 0.9% to 3.6%. The spinal cord compression by a hydatic cyst is a benign process but has considerable morbidity. It must be considered as a differential diagnosis in cases presenting symptoms and signs of spinal compression, particularly in endemic areas [1]. The spinal hydatic usually causes local or radicular pain according to the predominant site of the lesion, which can happen at the intramedullary region or intra/extra dural extramedullary, vertebral and paravertebral regions [2,3].
This study reports a spinal hydatid cyst compression case and will document a comprehensive review of spinal hydatidosis. After the surgical approach, the patient received albendazole 10–15 mg/kg/day for 4 months. In 4 months of follow-up, the case had no related complaints and her back and chest pain disappeared. Echinococcosis is a chronic zoonotic parasitic infection found worldwide but is most prevalent in subtropical and tropical regions. Its incidence/prevalence has not been established [4,5].
Of course, the symptoms and signs, such as paraesthesia, dysesthesias, motor deficits and back pain, will be related to how much compression is applied to the spinal cord. We will answer the following research question: How often does a hydatid cyst compress the spinal cord and how long should drug therapy be continued?
Literature Review
Search strategies
We comprehensively searched the electronic databases PubMed, MEDLINE, Research Gate, Scopus, Embase, Google Scholar and the English/Portuguese/Spanishlanguage medical literature.
Inclusion criteria
Peer-reviewed journals produced in English, Portuguese and Spanish articles published from January 31st, 2016, up to January 31st, 2025, the full text of the publication, type of publication: Systematic review, review articles, metaanalysis or empirical studies published in peer-reviewed scientific journals, compliance with the combinations of keywords: Treatment advances, targeted therapy, clinical features, pathobiology and the neurological manifestation were included.
Exclusion criteria
Articles published earlier than eight years, lack of full text of the publication, language of the publication different than English/Portuguese/Spanish, type of publication other than systematic review, meta-analysis, review articles or empirical studies published in peer-reviewed scientific journals, specific treatment protocol, co-morbidities along with the diseases affecting presentation or than that of the illness in review.
Key terms used for the search are “Echinococcus granulosus” (All Fields) OR “spinal Echinococcosis” (All Fields) AND “spinal cord compression by Echinococcosis” (All Fields) OR “compressive myelopathy by Echinococcosis” (MeSH Terms) OR “echinococcus myelopathy” (All Fields) OR “Eg’s response to drugs therapy.”
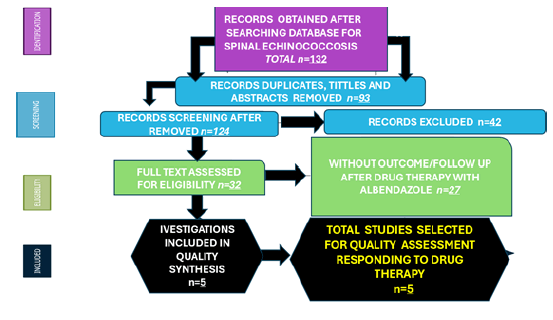
We identified 132 publications related to Eg; after removal of 93 articles due to duplication and other reasons, we reviewed the titles and abstracts of 124 publications. Twenty-seven records were excluded from the thirtytwo selected manuscripts because they did not document inclusion/exclusion criteria or follow up on the cases after the surgical approach. Still, they assess the outcome after six months of postoperative treatment with albendazole. A total of five were finally selected without considering the duration of the treatment. The PRISMA method used in the research methodology is depicted in Figure 1.
Figure 1: PRISMA Flow diagram with included publications.
27-year-old female presented with a 3-year history of signs and symptoms suggestive of spastic paraparesis.
Background history
The was last well in May 2022.
• June 2022: Pt started having back pain, which lasted about 1/12. She was attended to at a local clinic, where some meds were given and she somewhat improved.
• August 2022: She started developing issues with walking and needed crutches. This difficulty walking was associated with cramps and heat sensations. She also reported to have had urinary retention but no bowel issues.
• May 2023: She had a recurrence of backache and walking became even more complicated, so that she couldn’t manage with crutches anymore and needed a wheelchair.
• July 2024: She reports to have improved a bit and then managed to mobilise using crutches.
• May 2024: Recurrence of backache, urinary retention, bowel incontinence and paraesthesia’s in the lower limbs-burning sensations.
Past medical history
The patient was never diagnosed with TB previously and denied any knowledge of exposure or contact with anyone who has had TB. She has never had any injuries or traumas previously or a history of underlying disease. She admits to the use of traditional medicine for the management of her paraparesis. There is no surgical history of notes [6].
OBGYN
• Menarche at 18 yo.
• 3-4-day period, 28-day cycle with normal flow. LNMP- End June 2024.
• She hasn’t had a pap smear yet.
• P1A1: 2019: NVD: Female: Nil issues: The child is doing well. Contraceptive use: 3/12 depo.
Family history
• Both parents are alive and well.
• Four siblings: Two brothers and two sisters, all well.
Social history
• Unemployed patient. Relies on the childcare grant. The patient’s mother is also employed as a kitchen helper.
• Highest level of education-Failed matric.
Drug history: Never tried any ET-OH, tobacco or other illicit drugs.
Dietary history: Pt follows a mixed diet but has decreased red meat recently.
Exposure history: No evidence suggests any exposure to organic or inorganic irritants.
The patient did not have a pet.
Review of systems
She has had issues with epigastric pain, a sensation that something is moving up from her stomach to the mouth. She also reports heartburn. She also reports a dry cough for months that has been resolved recently. No issues with vision, smell or hearing (Supplmentry Table).
Investigations
The primary diagnosis was a spinal cord tumor, most likely an epidermoid one, since the cyst was not identified to be Echinococcosis with MRI primarily. Components of the cyst in sagittal cross-sections of T5 had caused damage and fracture of the thoracic vertebrae in this area. Second MRI of the thoracic spine showed a hydatid cyst and vertebral fracture. The microscopic finding was acellular lamellated and germinative layers accompanied by some scolices.
Blood workup: Grossly NAD.
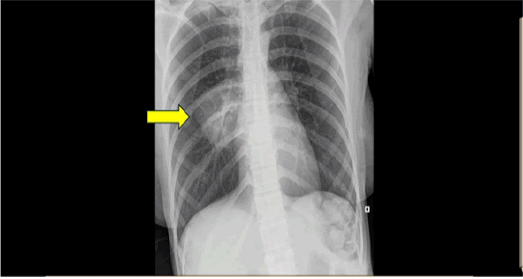
Chest X-ray revealed a right posterior pleural-based mass with a chondroid matrix at T7 to T9 (Figure 2).
Figure 2: CSF: Grossly NAD.
Case Presentation
CSF: Grossly NAD.
Ultrasound: Grossly NAD, but some thickened bladder wall.
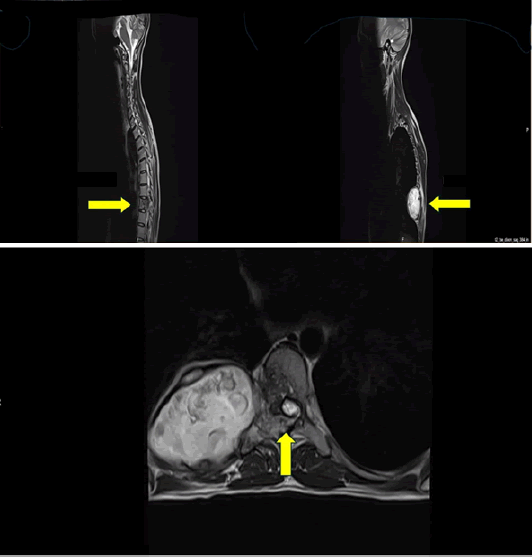
CT/MRI spine and chest: Preoperative MR images. Sagittal T2/T1-weighted image showing that a cystic lesion with septations has been embedded in T5; Sagittal enhanced T1- weighted image showing the cystic lesion wall and enhanced septa; Axial T2-weighted image showing compression of the spinal cord by the extradural cystic lesion (Figures 3 and 4).
Figure 3:PET scan of the whole body: Confirmed the compressive myelopathy by Eg.
Figure 4:Direct surgical approaches obliterated the mass, then the patient received six months of drug therapy with albendazole at the dose of 800mg PO daily and no signs of recurrence were detected.
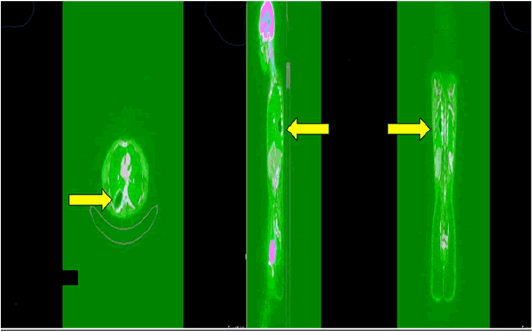
PET scan of the whole body: Confirmed the compressive myelopathy by Eg (Figure 5).
Figure 5: Bone Echinococcosis.
Direct surgical approaches obliterated the mass, then the patient received six months of drug therapy with albendazole at the dose of 800 mg PO daily and no signs of recurrence were detected.
Comments and final remarks
After an extensive, comprehensive search of the medical literature, we found only five patients with a similar history of present complaint, clinical features, pathological damage of the spine and similar outcome after drug therapy, which serve to confirm that this presentation is uncommon.
Table 1 summarizes the most relevant information obtained from the patients presenting cord compression by Eg in the current review. We confirm the number of patients reported to the medical literature presenting this pathological condition from January 31st, 2016, to January 31st, 2025, concluding that this process is not quite frequent.
Other authors from five released publications have documented that the gold standard therapy for hydatid cysts is surgery, which removes the whole cyst, followed by six months of pharmacotherapy with albendazole, plus praziquantel plus nitazoxanide, as we got the same results as well. The same investigators also suggested that in cases where the clinical diagnosis is doubtful of spinal Echinococcosis, the aspiration or biopsy ofthe cyst must not be performed due to the high risk of diffusion/anaphylaxis/dissemination of the infection that might happen [7]. Other authors have considered hydatid disease as a fatal zoonosis that could endanger human health worldwide, mainly in pastoral areas, semi-pastoral areas and semi-agricultural regions and where animal husbandry has been created [8]. On the other hand, other investigators have established that there are two primary forms of human infection with Echinococcosis, such as alveolar Echinococcosis and cystic Echinococcosis, with cystic Echinococcosis being the commonest one, which is known as Echinococcus granulosus (Eg). By analysing the phylogenetic relationship of Eg, the G1-G3 genotype of Eg was classified as G4 genotype as E. equinus, Eg sensu stricto, G5 genotype as E. ortleppi, Eg lion strain as E. felidis, G6-G10 genotype as E. canadensis [8,9].
Soon after Echinococcus infect a person, one or more cysts can grow primarily in the liver and lungs and often in kidneys, central nervous system, muscles, spleen, eyes and occasionally in the bones (2% to 5%). We report a case of extradural Eg causing paraparesis in the absence of clinical history and exposure. Imaging and clinical manifestations can accumulate more experience and improve the understanding of Eg spinal bone lesions [10].
It has been grossly estimated that there are more than one million patients with Echinococcosis all over the world and each year, there are approximately two hundred thousand new cases of cystic Echinococcosis [1]. Bone Echinococcosis is seen in about 2% of Echinococcosis, while spinal Echinococcosis accounts for about 50% of patients presenting osteoechinococcosis. Spinal cord compression is quite common in spinal Echinococcosis, accounting for 40% to 70% of overall cases [11]. Hydatidosis is listed as a local zoonotic parasitic disease of the livestock breeding population. It is an occupational disease with the features of occupational damage in the epidemic area and it is a widespread and frequently occurring disease of religious or ethnic tribes engaged in animal husbandry [12]. The definitive hosts of Eg are wild carnivores and dogs, such as jackals and wolves and they must rely on two mammalian hosts to complete the life cycle.
| Abbasi, et al. | 61/M | Persistent and severe low back pain | MR: Expansile heterogeneous lesion within the sacral bone with paravertebral and disc involvement CT: Expansile lytic lesion with areas of cortical disruption in the sacral bone |
Uninoculated lytic lesion with minimal soft tissue extension |
| Gennari, et al. | 25/F | Backache, paravertebral tumefaction and slight weakness | MR: Multiple cystic lesions invading the spinal canal producing spinal cord compression at level T9 CT: Right costovertebral destruction of T9 vertebra |
Whole extradural cyst |
| Unal et al. | 43/F | Left leg pain and fluid leakage from a cutaneous fistula on the left hip | MR: Heterogeneous low- signal intensity sacral lesion CT: Lytic lesions in bilateral wings of the S1 vertebra |
The lesion was in the vertebral body at S1 level and extended to the foramen and the paravertebral muscle |
| Vizcarra, et al. | 14/M | Progressive hypoesthesia | MR: Destruction and compression of L5 to S2 CT: Multilocular cystic tumor of L5 to S2 vertebrae |
Multiple thin- walled hydatid cysts, infiltrated in the bone and dural sac (L5-S2) |
| Cavus, et al. | 41/M | Paraplegia with urinary and faecal incontinence | MR: Multiseptated lesion extending from the right paravertebral region to the midline at the T10- T11 level CT: Narrowing of the intervertebral disc space, and destruction in the end plates at the T10-T11 level |
Cystic mass compressing the cord |
| Jacquier, et al. | 35/F | Impaired sensation in both legs | MR: Lobulated lesion of the 9th thoracic vertebra with an epidural component |
Cystic lesion in T9 vertebra involving spinal canal |
| Mansfield, et al. | 38/M | Chronic lower back pain | MR: Vertebral body destruction of the L4 vertebra with multiple surrounding cysts |
N/A |
| Meinel, et al. | 75/F | Atypical low back pain | MR: Multilobulated osteolytic cystic mass in the lumbar and paravertebral region, originating from the L3 and L4 vertebrae CT: Mult cystic lesion without calcifications of the paravertebral mass |
Extradural granulation and purulent fluid at L1- L4 with destruction of laminae |
| Kandwal, et al. | 30/M | Low back pain with radicular pain in the left lower limb | MR: bony destructive lesion involving the left half of the L3 body, the pedicle and the transverse process CT: Osteolytic lesion with absence of L3 pedicle on the left side |
The lesion was extradural and predominantly confined to the L3 vertebra |
| Saha, et al. | 22/M | Backache with progressive weakness of both lower limbs | MR: Mixed hypodense and hyperdense epidural soft tissue mass lesion with few fluid intensities |
Extradural intraspinal lesion |
| Xia, et al. | 47/F | Back pain | Lesion located in T7-T9 |
N/A |
| 50/M | Back pain | Lesion located in L3-L5 |
N/A |
|
| 43/M | Headache | The lesions invaded the brain and T11-L5 |
N/A |
|
| 32/F | N/A | Spinal cord compression at T3-S5 level |
N/A |
|
| 69/M | Abdominal pain | Lesions located in spinal canal at L3-L5 level |
N/A |
|
| Majmundar, et al. | 38/F | Low-back pain, bowel incontinence as well as subjective lower-extremity weakness | MR: Polycystic mass extending from the pelvis into the epidural space from at L5–S1 level |
Epidural mass at L5–S1 level |
| Vizcarra, et al. | Seven male/ nine female | Low-back pain with spinal cord compression | The upper thoracic spine (T1–T4) in one patient, the mid thoracic spine (T5–T8) in eight, and the lower thoracic spine (T9– T12) in seven |
One intradural extramedullary case, two extradural cases, nine vertebral cases, and four paravertebral cases |
| Dkhissi et al. | 28/F | Weakness and numbness of the lower limb | MR: Multiple cysts at L3 level with extension into the spinal canal at L2 and L4 levels compressing the cauda equina and to the peri-vertebral soft tissue |
N/A |
| 34/F | Lumbar-radicular pain and functional impotence of lower limbs | MR: bony destructive lesion involving the left half of the L3 body, the pedicle, and the transverse process CT: Osteolytic lesion with absence of L3 pedicle on the left side |
N/A |
|
| Saul, et al. | 42/M | Chronic back pain | MR: lytic progression in T8 with high-grade constriction of the spinal cord |
The T8 vertebral body was inter- fused by white granular tissue |
| Çeviker, et al. | 63/M | Lost bilateral lower extremities strength, paraplegia immobilization, and swelling in the thoracolumbar region | In MRI thought to be metastasis, involving the dorsal colon, right pedicle and lamina, and soft tissue densities |
Hyperdense calcific foci the spinal canal in the T11 |
| Santo,s et al. | 22/M | Paraesthesia, numbness in the chest, lower limb paraparesis, and back pain in a sitting position | CT and MRI showed multiloculated cysts extending to the entire length of the second right costal arch, especially to the intrathoracic length of the second right costal arch, especially to the intrathoracic |
The lytic lesion was found on the body and posterior arch elements of the T2 vertebra and the posterior elements of the T1 and T3 vertebrae |
| Das, et al. | 35/M | Back pain and intermittent fever | Kyphosis in the D2–D6 and partial collapse of D4 were found in the X-ray result. hydatid cyst disease was confirmed in the D4 vertebra involving the paravertebral area |
In the paravertebral area, intact cysts were removed |
Table 1: Reported cases of spine hydatid cyst.
In contrast, the intermediate hosts are pigs, cattle, sheep and other cloven-hoofed animals, infecting larvae by consuming water and food contaminated by eggs or contacting canine animals. On the other hand, humans can be intermediate hosts of Eg. However, humans are usually the only victims and are not traditionally involved in the parasite’s life cycle [13]. Some habits related to natural burial and water burial with the participation of some ethnic minorities have been reported, where people may participate in the classic dog/ cattle life cycle [14,15].
As we mentioned before, the liver and lung, in that order, are the most common sites of infection by Eg in the human body. Clinical features are generally hidden depending on the location and size of the lesions. Therefore, the lesions caused by Eg are usually undetected until they are big enough to cause symptoms by mechanical compression/infiltration. Notwithstanding, the symptoms of Echinococcosis in the spine depend on the intensity of spinal cord compression. Nevertheless, some nonspecific clinical manifestations, such as sensory discomfort, pain, dysuria and others, can happen during the compression of the spinal cord [16]. Cavus and other collaborators have established that the MRI of the spine bone supports the assessment of the hybrid cyst of the vertebral body [17].
Where the cyst wall shows hypointense patterns of T2-weighted sequences and isointense patterns of T1- weighted sequences, the cyst consists mainly of waterfree, with the appearance of hyperintense to T2-weighted sequences as we found in our patient. In our case, we also found ring and septa enhancement on post-contrast T-1-weighted sequences. Therefore, we need to make a confident differential diagnosis with other similar imaging presentations like spinal tuberculosis, haemangioma, neurogenic tumours, tumour metastasis or an aneurysmal bone cyst. However, it is not easy to differentiate between them. We made the differential with spinal tuberculosis based on its characteristic osteolytic destruction of the vertebral body, usually associated with osteonecrosis, with disappearance or narrowing of the intervertebral space and sometimes accompanied by a cold abscess beside the vertebral body. In some patients, the cystic hyper-signal on fat-suppressed T2WI sequence supports the diagnosis of spinal Echinococcosis.
On the other hand, metastatic tumours of the spine usually do not present as T2 high signal vesicles and show typical features of multiple vertebral lesions. In contrast, spinal Echinococcosis typically does not present multifocal lesions. To differentiate vertebral haemangiomas, we investigate the percentage of fat in the vertebral haemangiomas, which determines their signal characteristics on MRI. On top of that, vertebral haemangiomas show low-signal intensity on T2WI, hyper or hypo-signal intensity on T1WI and are frequently asymptomatic. On CT of the spine, we look for the trabecular appearance of the bone, which helps separate from Echinococcosis. To distinguish neurogenic masses in the spinal canal, we considered that they usually grow eccentrically around one side of the foramen of the vertebral bone and are dumbbell-shaped, extending near or near the spinal canal. The dumbbell-like features help differentiate it from a spinal hydatid cyst. A lobulated neural arch mass that extends into the vertebral body is present to distinguish the aneurysmal bone cysts.
Based on our literature search, we concluded that the use of albendazole should be limited to six months up to one year to prevent the recurrence of hydatid cysts. Unfortunately, patients who were treated with anti-echinococcosis drugs for life could not avoid relapse [18]. As Eg is a systemic disorder with locally focal clinical manifestations, in some cases where the therapeutic effect evaluation and the definition of cyst inactivity cannot be reached, a course of anti-echinococcosis therapy in the postoperative period may be recommended. If a cyst rupture happens during the surgical approach, “lifelong medical treatment and followup” is mandatory [18]. For example, infection leads to high expenses and economic losses to veterinary medicine and medical care. Therefore, vaccination could be the best strategy for preventing hydatidosis [19].
Discussion
Bone echinococcosis
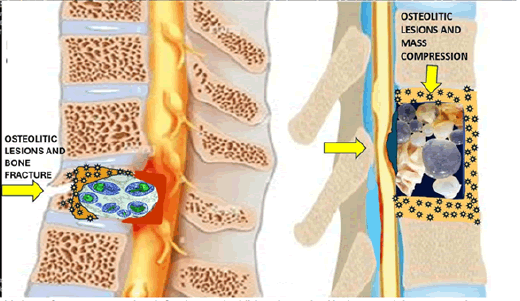
Bone Cystic Echinococcosis (BCE) is one of the most dangerous and complex Echinococcosis. As we defined before, Echinococcosis or hydatid disease, is an endemic disorder that affects multiple regions worldwide mainly where agriculture and cattle farming play a significant role, especially for the herdsmen in the endemic areas which is caused by an infection with the dog tapeworm Echinococcus, that invades humans either by ingesting contaminated food or through direct contact with dogs, affecting primarily the liver and lungs, but in our patients presenting as BCE at the spine bone with associate compression of the cord [20]. In case where the parasite invades the spine, it grows slowly in the bone tissue, disseminates along the trabecular cancellous bone and reaches the bone through the medullary canal. The result is infiltration of vesicles of different sizes without an outer membrane. Bone involvement in hydatid disease is relatively uncommon, representing about 0.5% to 2.5% of human hydatidosis cases. Therefore, its diagnosis may be delayed and often mistaken for other common pathologies, such as tumor or bone infections [21,22]. The clinical manifestation of bone Echinococcosis, also known as “white cancer of the bone,” is variable and often absent for prolonged periods, making this pathological process hard to detect until it reaches large lesions at an advanced stage, following symptoms and signs like pain, deformities or pathological fractures, as it graphically represented in Figure 5A.
This bone fracture, secondary infection and additional vertebral lesions result in compressive myelopathy surrounded by multiple cystic formations, which can be seen on imagenology as hypointense on T1-weighted images and hyperintense on T2-weighted images, without enhancement postcontrast. Therefore, multi-vesicular appearance suggests intraosseous hydatid cysts. The shape of the cyst is round, well-defined shadow, watery. In contrast, the daughter cyst in the polycystic mother cyst is a round, low-density shadow in the septum, sometimes with calcification in the cyst wall or the cyst. These imaging findings usually show cystic dilatancy, septal or irregular bone destruction and the lesions’ size can vary and lead to bone expansion with cortical involvement. Sometimes, the represented osteolytic areas have poorly defined margins [23]. Apart from the pathological fractures, there is an extension to the adjacent soft tissues, mimicking a tumoral process as shown in Figure 5B. MRI is also mandatory for detecting early recurrences of hydatid cysts after the surgical approach if antiparasitic drugs are not administered. The pathological appearance of the hydatic cysts is shown in Figure 5B.
The serological test can be a valuable diagnostic tool for hydatid disease, but it sometimes shows false positive and false negative results; therefore, it cannot serve as the best early diagnostic tool for mass screening in areas of endemicity [24]. We hypothesised that protoscoleces invade the human body and through blood flow, parasitise different organs, including cancellous bone tissue with cystic formation which can fracture bone tissue and spread to invade exoskeletal structures. We consider that when the growing cysts are big enough, they can cause bones to atrophy and they move into the less-resistant microstructures like the bone canal; they erode and replace bone trabeculae, destroying the bone. When the cystic lesion is large enough, it compresses the blood vessel supplying the bone tissue, leading to local swelling of the tissue, secondary local infection and ischemic necrosis activating the production of osteoclasts, causing multifocal osteolytic lesions as it is represented in Figure 5A-5B. That cystic invasion decreases the host immunity and activates the local microglia polarisation with proliferation of proinflammatory and anti-inflammatory elements causing direct cord damage via programmed cell death. Due to a dense regional vascular network and rich blood supply in the thoracolumbar segment of the spine, E. G. infiltrate vertebral cancellous bone via the vertebral artery and produce a bone marrow cavity toward the epiphyseal plate and articular cartilage [25-28]. We also speculate that most infected tissue does not attack the intervertebral disc due to the periosteal barrier despite the progressive sclerotic cysts compressing the pedicle, vertebral body and lamina. Forthcoming investigation results will support, modify or delete our hypotheses.
Conclusion
In conclusion, most lesions present high signal intensity on T2WI and are well-defined. The presence of signs of fluidfluid level is beneficial for distinguishing aneurysmal bonecysts from spinal compression by hydatid cysts. In our case, Enzyme-Linked Immunotransfer Blot (ELTB) and ELISA confirmed the diagnosis of cystic Echinococcosis. The clinical features of spinal cord compression by hydatic cyst due to radiculopathy, myelopathy or cauda equina syndrome are strongly related to the lesion size, spinal level, location and inflammation caused by cyst degeneration.
Author Contributions
Both authors contributed equally to the conceptualisation, methodology, writing-review, editing, supervision, original draft, review and editing.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Consent
Written informed consent was obtained from the patient to publish this report and images.
Data Availability Statement
All data of our present case are available in the manuscript. For additional information, please get in touch with the corresponding author.
Acknowledgments
We thank Dr Sibi Joseph for the summary discharge of this patient.
References
- Z. Alireza, S. Mohammadreza, B. H. Biazar, N. M. Noosha Samieefar, M. Akhlaghdoust, Spinal hydatid cyst initially diagnosed as spinal tumor: A case report and review of the literature, Clin Case Rep, 11(2023):e7244.
- A. Salduz, L.O. Koyuncu, F. Dikici, U. Talu, Long-term result of treatment for paraspinal and extradural hydatid cyst: A case report, Acta Orthop Traumatol Turc, 43(2009):267-271.
- A. Neumayr, F. Tamarozzi, S. Goblirsch, J. Blum, E. Brunetti, Spinal cystic echinococcosis–a systematic analysis and review of the literature: Part 2. Treatment, follow-up and outcome, PLoS Negl Trop Dis, 7(2013):e2458.
- B. Zhang, L. Zhang, H. Zhou, J. Tian, J. Wang, Progressive compressive myelopathy induced by a rare primary isolated thoracic vertebral hydatid cyst: A case report, Medicine, 100(2021):e25177.
- B. Monge-Maillo, M. Olmedo Samperio, J.A. Pérez-Molina, Osseous cystic echinococcosis: A case series study at a referral unit in Spain, PLoS Negl Trop Dis, 13(2019):e0007006.
- H. Safari, S. Mirzavand, A. Rafiei, M. Beiromvand, Twenty-six years of involvement with cystic echinococcosis: A case report, J Med Case Reports, 15(2021):1-4.
- G. Das, S.N. Nanda, N.K. Sahu, D.S. Kumar, B.P. Patro, Hydatid cyst of dorsal spine masquerading as tubercular infection: A case report and review of literature, Asian J Neurosurg, 16(2021):886-889.
- M. Prabhakar, A.J. Acharya, D.R. Modi, B. Jadav, Spinal hydatid disease: A case series, J Spinal Cord Med, 28(2005):426-431.
- B. Abbasi, R. Akhavan, F. Seilanian Toosi, A man with disabling low back pain: Echinococcus of the sacrum, Int J Infect Dis, 49(2016):68–70.
- A. Gennari, F. Almairac, S. Litrico, Spinal cord compression due to a primary vertebral hydatid disease: A rare case report in metropolitan France and a literature review, Neurochirurgie, 62(2016):226–228.
- T.R. Meinel, B. Gottstein, V. Geib, Vertebral alveolar echinococcosis-a case report, systematic analysis, and literature review, Lancet Infect Dis 18(2018):e87–e98.
- G. Cavus, V. Acik, E. Bilgin, Endless story of a spinal column hydatid cyst disease: A case report, Acta Orthop Traumatol Turc, 52(2018):397–403.
- S.T. Mon, Y. Li, S. Shepherd, Recurrence of chest wall hydatid cyst disease involving the thoracic spine in an Australian patient, J Clin Neurosci, 30(2016):132–136.
- N. Milhau, E. Almouazen, S. Bouteille, In vitro evaluations on canine monocyte-derived dendritic cells of a nanoparticles delivery system for vaccine antigen against Echinococcus granulosus, PLoS One, 15(2020):e0229121.
- B.S. Mansfield, K. Pieton, S. Pather, Spinal cystic echinococcosis, Am J Trop Med Hyg, 100(2019):9–10.
- V.M. Unal, N. Ozdemir, A. Karadag, Primary sacral hydatid cyst causing cutaneous fistula, J Coll Physicians Surg Pak, 27(2017):311–312.
- M. Vizcarra, M. Mujica, V. Sánchez, An adolescent with lumbosacral instability due to the presence of a hydatid cyst: A case report, Rev Peru Med Exp Salud Publica, 34(2017):126–131.
- M. Jacquier, L. Piroth, Vertebral hydatidosis, N Engl J Med, 379(2018):e5.
- P. Kandwal, G.Vijayaraghavan, B.N. Upendra, Single-stage vertebrectomy for hydatid disease involving L3 vertebra: Five year follow-up, Neurol India, 66(2018):1499–1501.
- A. Saha, K. Saha, V. Agrawal, Isolated spinal epidural hydatid disease: A diagnostic challenge in a needle core biopsy, Indian J Pathol Microbiol, 61(2018):640–642.
- X.I. Yong, J.U. Yan, L.I. Jin Ping, C.H. Long Yi, Common spinal parasites, Turk Neurosurg, 29(2019):409-413.
[Crossref] [Google Scholar] [PubMed]
- N. Majmundar, P.D. Patel, V. Dodson, A. Tran, I. Goldstein, et al. Parasitic infections of the spine: Case series and review of the literature, Neurosurg Focus, 46(2019):E12.
[Crossref] [Google Scholar] [PubMed]
- Y. Dkhissi, B. Alami, M. Haloua, M.Y. Lamrani, M. Boubbou, et al. Unusual sites of hydatid disease: Report of two cases of dumbbell formations, Pan Afr Med J, 36(2020):109.
[Crossref] [Google Scholar] [PubMed]
- D. Saul, M.T. Seitz, L. Weiser, S. Oberthür, J Roch, et al. Of cestodes and men: Surgical treatment of a spinal hydatid cyst, J Neurol Surg, 81(2020):86-90.
[Crossref] [Google Scholar] [PubMed]
- J.K. Sharma, V. Tandon, N.A. Marathe, Y. Agrahari, A.R. Mallepally, et al. Hydatid cyst of the spine: A rare case report and review of literature, J Orthop Case Rep, 10(2020):57.
[Crossref] [Google Scholar] [PubMed]
- R.C. Santos, G.J. da Nobrega Danda, A.M. Junior, G.R. de Amoreira, Spinal hydatid cyst as cause of neurological injury in a patient from Brazilian amazon region, Radiol Case Rep, 17(2022):2238-2242.
[Crossref] [Google Scholar] [PubMed]
- G. Das, S.N. Nanda, N.K. Sahu, D.S. Kumar, B.P. Patro, Hydatid cyst of dorsal spine masquerading as tubercular infection: A case report and literature review, Asian J Neurosurg, 16(2021):886-889.
[Crossref] [Google Scholar] [PubMed]
- N. El Mahi, S. Hajar, M. Amal, H. Karim, Z. Hamid, et al. Femoral hydatid cyst: A rare localisation of bone echinococcosis: A case report, Radiol Case Rep, 20(2025):1691–1694.
[Crossref] [Google Scholar] [PubMed]
Copyright: © 2025 Lourdes de Fatima Ibanez Valdes, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.