Research: Journal of Drug and Alcohol Research (2023) Volume 12, Issue 2
Poly Pharmacy and Potential Drug-Drug Interactions among Elderly People: Hospital Based Cross-Sectional Study
Bedilu Linger Endalifer1*, Yehualashet Teshome Wondemkun1, Habtemariam Alekaw Habteweld1, Abyou Seifu Ambaye2, Yenesew Wudu Ejigu3 and Abate wondesen Tsegie12Department of Pharmacy, Mizan-Tepi University, Ethiopia
3Department of Pharmacy, Wollo University, Ethiopia
Bedilu Linger Endalifer, Department of Pharmacy, Debre Birhn University, Ethiopia, Email: lingerendalifer@gmail.com
Received: 01-Mar-2023, Manuscript No. JDAR-23-97924 ; Editor assigned: 03-Mar-2023, Pre QC No. JDAR-23-97924 (PQ); Reviewed: 17-Mar-2023, QC No. JDAR-23-97924 ; Revised: 22-Mar-2023, Manuscript No. JDAR-23-97924 (R); Published: 29-Mar-2023, DOI: 10.4303/JDAR/236228
Abstract
Introduction: Patients with advanced age and with 4 chronic diseases were the most likely to use highest health care services. Polypharmacy and pDDIs are independently associated and consequences significant health burden in older patient. The objectives of the study were to study polypharmacy and pDDIs among geriatric patients on follow-up.
Design, setting and participants: Hospital based prospective cross-sectional study design was conducted at Dessie comprehensive specialized hospital which is located in Ethiopia from November 01, 2021 to February 2022. Finally 210 patient charts fulfills the inclusion criteria were enrolled. Patient demographic information, patients’ medical conditions and medication-related information were collected by using structured data abstraction tool. Polypharmacy was considered if the patient took 5 or more drugs together. Micromedex® drug interaction checker was used to identify potential drug-drug interactions.
Result: In this study, medical records of 210 patients with chronic disease conditions on follow up were collected. The mean age was 70.78 ± 5.996 years. The men number of drugs prescribed was 3.40 ± 2.86, the magnitude of polypharmacy (5 or more drugs) were 22.4% (47). Significant association was observed between polypharmacy and patients on cardiovascular disease and infectious disease. Atleast one potential drug-drug interactions observed in 144 (68.6%) patients with an average of 25.2 ± 38.6 and 458 total potential drug-drug interactions were identified. Majority of potential drug-drug interactions 264 (57.6%) were moderate and the rest 194 (42.4%) were major in nature. Pharmacodynamics 238 (52%) mechanism of interaction accounts the highest frequency. Age, sex, and number of drugs prescribed showed significant contribution for the occurrence of potential drug-drug interactions.
Conclusion: Polypharmacy and potential drug-drug interactions are higher in magnitude and might consequence significant health and economic burden.
Keywords
Polypharmacy; Drug-drug interaction; Elders
Introduction
Prevalence of people aged 60 years and above will be 1 in 6 in 2030 and by 2050, will doubles (2.1 billion). The world’s 65 years and-older population will twofold by the year 2050. Ageing is associated with biological changes, physiological changes, and numerous medical conditions general geriatric syndromes which is described as common health problems include frailty, functional impairment, falls, malnutrition, depression, poly pharmacy, and cognitive impairments, hearing loss, vision problems, back pain and osteoarthritis, chronic obstructive pulmonary disease, diabetes mellitus, depression and dementia re common diseases.
There is no standard definition for polypharmacy, the most commonly used once is prescribing of 5 or more medications at once, this definition includes over-the-counter, prescription and/or traditional and complementary medicines. Numerical definition of polypharmacy may not be the exact indictor for elders because of direct relation of number of drugs with number of comorbidities. Polypharmacy is not always inappropriate, may be indicted for prophylaxis of drug side effects, increased disease control for comorbidities and for minimization of several symptoms but there may be pronounced demerits of higher risk of drug-drug interaction, higher incidents of adverse drug reaction, risk of non-adherence, medication error risks and higher costs for the patient [1].
Because of multiple health conditions in aged patients, the use of several medications is unavoidable. Drug therapy for elderly requires special concern on the age related changes in drug pharmacokinetics and sensitivity profile [2]. Due to a reduced in renal function; decrease in water content of the body, increase fat content; the distribution volume of hydrophilic drugs may reduce in the elderly, resulting in increased plasma concentrations. Whereas the distribution volume of lipophilic drugs is increased, their plasma concentrations may decrease, as age increase, people usually have more health problems that lead to more medications than younger people do. Because of this, elders are more likely to develop serious drug-drug interaction. Having more than one disease and polypharmacy is a major problem for elder patients. Healthcare costs are greatly increased, due additional increased in specialist physician, emergency department visit, and admissions as chronic condition pronounced. As a result, older patients prone for deterioration of quality of life, more expenditure, poor medication adherence, symptom control and optimal care [3].
A drug-drug interaction is a change in the action of a drug caused by concomitant administration with another drug. The risk of drug-drug interaction increases with the number of drugs prescribed. Patient morbidity from drug interactions can be addressed. Harm may result from either an increase in the drug’s toxicity or a decrease in its therapeutic efficacy [4].
Older people who live at home have a high prevalence of polypharmacy and potential Drug-Drug Interactions (pDDIs). In older persons with CVD, polypharmacy, hyper- polypharmacy, and significant pDDIs are particularly common. In order to avoid hazardous drug responses and poor health outcomes, clinicians should carefully monitor patients’ drug records and modify therapy as necessary.
Polypharmacy and comorbidities were contributory factors for hospital admissions [5]. At least one pDDI is present in two thirds of aged people. They have a 4 times increased chance of developing pDDIs, elderly individuals taking 5 or more drugs need to be closely monitored. A crucial part of a pharmacist’s job is to identify and avoid hazardous pDDIs, and the clinical pharmacist is responsible for monitoring potential DDIs and adjusting dosage or therapy as necessary. Polypharmacy was found to be a significant predictor of pDDIs in the study. In high-risk populations like senior patients, rational prescribing and the use of information technology can help to improve pharmaceutical safety [6].
There is a high possibility of drug interactions with a risk of adverse events in vulnerable elderly individuals. The most important drug interactions were observed with drugs frequently used in clinical practice. Patients at risk for drug interactions should be closely monitored and awareness raised those over-the-counter drugs may cause drug interactions [7]. Drugs acting on the cardiovascular system, including low dose aspirin, diuretics, angiotensin converting enzyme inhibitors, calcium channel blockers, beta blockers and digoxin; were more often than not involved in potential drug interactions. Patients with advanced age and with 4 chronic diseases were the most likely to use highest health care services. Polypharmacy and pDDIs are independently associated and consequences significant health burden in older patient. The objectives of the study were to study polypharmacy and pDDIs among geriatric patients on the outpatient department [8].
Methods and Materials
Description of study setting
The study was conducted at Dessie comprehensive specialized hospital which is located in Ethiopia, Amhara regional state, South Wollo Zone, Dessie town. It is a referral and teaching hospital for students of Wollo University and different private colleges. It serves for large number of people from the surrounding zones and nearby regions for routine health care services for the city community and other referral cases from different regional states. Medical referral clinic which gives follow-up care for chronic patients is among variety of services delivered by the hospital.
Study design, sample size and data collection
A hospital based prospective cross-sectional study design was employed from November 01, 2021 to February 28, 2022. All patients aged 65 years and above attending the medical referral clinic were study population. Total of 540 patient cards are observed by data collector. Those patients with incomplete medical and medication information and patients prescribed only one drug were excluded. Finally 210 patient charts were selected during the study period (Figure 1). Patient demographic information (age and sex), patients’ medical conditions (comorbidity, number of drugs prescribed, and diagnosis) and medication-related information, OTC medication use has collected by using pre-designed data abstraction tool. Herbal medication use was not included since difficult to identify the exact constituents of the plants. The questionnaires did not contain information on the cause or date of prescription, dosage or regularity of prescription drugs. As a consequence, the total number of drugs reported is counted in this study. Micromedex® drug interaction checker was used to identify potential drug-drug interactions.
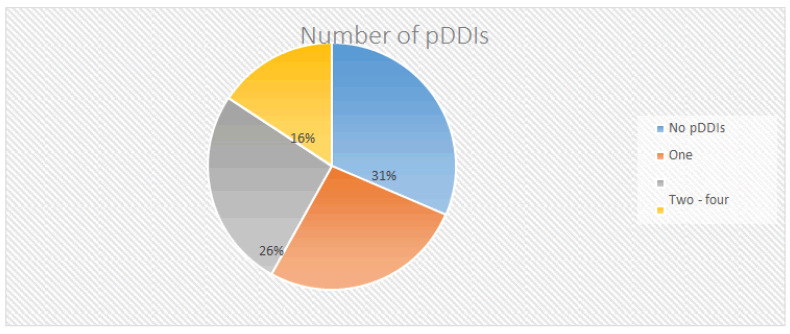
Figure 1: Flow diagram of selection of study charts.
Polypharmacy
However there is no accepted standard definition of polypharmacy, the investigators used prescriptions of 5 and more drug at a time as polypharmacy. Therefore, for this study, the polypharmacy status was divided into 2 groups: Non-polypharmacy prescription of 1 to 4 medications and polypharmacy.
Potential drug-drug interactions
The pDIs were evaluated by means of computerized verifications available online on micromedex Internet. The website categorized pDID among all prescription medications severity, mechanism of interaction onset of action and documentation level of evidences. Based on severity, mild/minor drug interaction have little clinical significance therefore the interaction is not likely to have clinical relevance whereas moderate interactions are clinically relevant, used only in special circumstances where close supervision is necessary; it may result in exacerbation of the disease of the patient and/or a change in the therapy. Severe drug interactions are extremely clinically important and life threatening and/or they require medical treatment or an intervention to minimize or to prevent the severe adverse effects. Mechanisms of drug Interactions related to either pharmacokinetics or pharmacodynamics of the drugs [9].
Inclusion/exclusion criteria
Prescription records of elderly patients of age 65 and above who are on flow up at least on 2 drugs were incorporated whereas prescription charts with incomplete information and prescription with only topical preparations were excluded.
Statistical analysis
The data was entered into EPI-data version 4.2.0.0 and analyzed using Statistical Package for IBM Social Sciences (SPSS) version 25. The analysis result of continuous variables was described in mean and standard deviation for (age), while categorical variables (gender) were expressed in percentages. Potential associations or relationships between the predictor variables (gender, Comorbidity, age and diagnosis) and polypharmacy were determined with the Chi-square test of associations. Univariable binary logistic regression analysis was performed to relate each independent variable with drug-drug interaction. Odds Ratio (OR) with a 95% confidence interval was also calculated for each variable with the respective P-value to identify the association.
Results
Socio-demographic and related profiles
In this study, medical records of 210 patients with chronic disease conditions on follow up were collected. The mean age was 70.78 ± 5.996 years. Half of the patients (n=107; 51.0%) were between 65 to 69 years of age and males (n=107; 51.0%). Majority of the patients encountered 2and more diseases ((n=100; 76.2%) with 2.86 ± 1.811 a mean number of diseases per patient. About two-thirds of the patients received 3 and above drugs (65.4%), having men number of drugs 3.40 ± 2.86. the most common identified conditions were cardiovascular disease ((n=167; 79.5%) (Table 1).
| Variables | Characteristic | Frequency | (%) |
|---|---|---|---|
| Gender | Male | 107 | 51 |
| Female | 103 | 49 | |
| Age | 65-69 | 107 | 51 |
| 70-74 years | 63 | 30 | |
| 75 and above | 40 | 19 | |
| Comorbidity | Mean ± SD | 70.78 ± 5.996 | 19 |
| No | 50 | 23.8 | |
| Yes | 160 | 76.2 | |
| Number of comorbidity | One | 50 | 23.8 |
| Two | 100 | 47.6 | |
| three and above | 60 | 28.6 | |
| Mean ± SD | 2.86 ± 1.811 | 28 | |
| Number of drug | two drug | 77 | 36.7 |
| three and four | 86 | 41 | |
| five and above | 47 | 22.4 | |
| Mean ± SD | 3.40 ± 2.86 | 32 | |
| Disease condition | Cardiovascular disease | 167 | 79.5 |
| Endocrine disease | 129 | 61.4 | |
| Respiratory disease | 11 | 5.2 | |
| Neurologic disease | 17 | 8.1 | |
| Ophthalmic disease | 12 | 5.7 | |
| Infectious disease | 7 | 3.3 |
Table 1: Socio-demographic and clinical profiles (n=21).
Prevalence and revision of associations between variables of polypharmacy and geriatric patients
In this study, 210 patient charts were evaluated, the magnitude of polypharmacy (5 or more drugs) were 22.4%. From 47 poly pharmacy patients, 24 were males. Sex have no significant association for the occurrence of polypharmacy (chi-square; χ2=0.157, p=0.924, phi=0.027). Significant association was observed between polypharmacy and patients on cardiovascular disease (chi-square; χ2=24.492, p=0.000, phi=0.342) and infectious disease (chi-square; χ2=10.762, p=0.005, phi=0.226). All poly pharmacy patients encounter 2 or more disease condition (comorbidity), the prevalence of polypharmacy as significantly high with comorbid disease condition (chi-square; χ2=51.267, p=0.000, phi=0.494) (Table 2).
| Variables | Characteristic | Poly pharmacy | No polypharmacy | χ2 | P. value, Phi. Value |
|---|---|---|---|---|---|
| Gender | Male | 24 | 83 | 0.15 | 0.924, 0.027 |
| Female | 23 | 80 | 3.56 | 0.924, 0.027 | |
| Age | 65-69 | 27 | 80 | 7.95 | 0.093, 0.195 |
| 70-74 | 14 | 49 | 9.6 | 0.099 | |
| >=75 | 6 | 34 | 7.8 | 0.882 | |
| Comorbidity | Yes | 47 | 113 | 51.2 | 0.000, 0.494 |
Table 2: The associations between variables of poly pharmacy and geriatric patients.
Prevalence, mechanism and nature of drug-drug interaction
From 210 patients chart reviewed 144 (68.6%) patients encountered at least one potential drug-drug interaction. An average of 25.2 ± 38.6 and 458 total potential drug-drug interactions were identified. Each participant were exposed to 2.18 ± 2.90 potential drug-drug interactions. Majority of potential drug-drug interactions 264 (57.6%) were moderate and the rest 194 (42.4%) were major in nature. Pharmacodynamics 238 (52%) mechanism of interaction accounts the highest frequency the second most frequent interaction was pharmacokinetics 111 (24.1%) and 4 (0.9%) drug interactions both PK and PD were probably my occur, The rest, 105 (23%) documented as Unknown mechanism of interaction.
Potential drug-drug interactions were higher on patients prescribed 3 and 4 drugs, but those patients only on to 2 drugs were less prone to PDDIs (Figure 2).
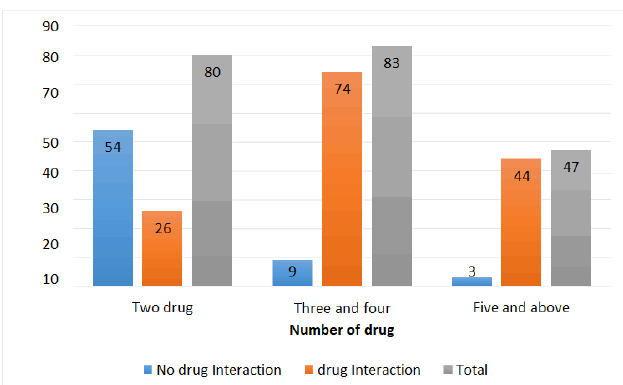
Figure 2: Drug-drug interaction with number of prescribed drugs.
Association between potential drug-drug interaction and different factors
The variables associated with an increased risk of potential DDI on univarate analysis were age, sex, number of drugs, number of comorbidity, neurological, endocrine, cardio-vascular and ophthalmic disorders he associated with the presence of pDDIs. By further analysis by Multivariate logistic regression only age, sex, and number of drugs showed significant association. Interestingly; the risk of potential DDI was not influenced by number of comorbidity, cardiovascular, neurologic, endocrine and ophthalmic disorders based on this finding.
Discussion
Pharmacotherapy in patient care and disease management is essential for improving optimal health. In this study medical charts of elderly (aged 65 year and above) people with chronic diseases were examined and analyzed for polypharmacy and pDDI at DCSH focusing on mechanism, severity and nature of drug-drug interactions: Most commonly involved drugs and the factors he significant contributions were determined. Both polypharmacy and potential DDI were significant in older patients.
In this study, medical charts of elderly (aged 65 year and above) patients on chronic follow up were examined and determined for the magnitude of polypharmacy and potential drug-drug interactions. In addition, the severity and mechanisms of drug-drug interactions, most commonly involved drugs and the most frequently occurred potential drug-drug interactions were analysed. The relationship between potential DDI, polypharmacy and age is well identified in this study. For this, study, polypharmacy is defined as a prescriptions of 5 or more different drugs at a time. In this study, 22.4% of the elderly patients used at least 5 different therapeutic classes. On the other hand 68.6% patients encountered at least one potential drug-drug interaction.
This magnitude of polypharmacy was in range with previous studies done in India (22.93%) and in Ethiopia 24.1%. Our findings are significantly lower as compared to results of other studies which range from 33% to 95%. This variability in magnitude in previous studies might be due to several reasons. The first justification might be difference study area (setting of study) conducted; being multi-center and inclusions of admitted patients in the previous study whereas only ambulatory patients reincluded in the current study. It is scientifically proved that hospital and prevalence of polypharmacy have significant association. The second possibly rationality might be due to variations in clinician practices across different countries and age variations during recruitment of study participants. The third possible reason is applying different definitions of poly pharmacy. For sum up, the prevalence of polypharmacy varies widely according to the age group, definition used, and study setting and study period.
Similarly with the previous studies, there was no correlation between age group and number of drugs being used. Factors such as comorbidity (more than one disease condition), cardiovascular and infectious diseases have potential to increase the magnitude of polypharmacy. This is supported by other study which concluded that, number of comorbidities, older age, and CVD were associated with polypharmacy.
Potential drug interactions observed in the current study were higher as compared (39.46%). This finding was lower as compared to other studies done in Ethiopia [10]. This study reported that as number of interaction increases, the prevalence decreases, the highest 27% of patients exposed for single drug interaction, 26% exposed with range of 2 to 4 and 16% for 5 and more pDDIs. This is justified by the previous reports stated that ≥ 6 pDDI accounts 6.20% and 1–2 pDDI, was 20.24%).
The identified drug interactions were classified by severity, Mechanism of interaction, onset of action and possible outcomes. The highest percentage of pDDs identified based on severity was moderate (57.6%). Similar result was reported which stated as moderate (84.3%) interaction accounts the highest prevalence. Among moderate interactions, ASA+Enalapril prescribed 36 times; Aspirin may diminish the vasodilator and hypotensive effects of ACE inhibitors. The probable mechanism is by inhibition of cyclooxygenase enzyme, and prostaglandin-mediated hemodynamic effects of ACE inhibitors. Therefore patients on long-term therapy of combination should be on regular monitoring (blood pressure and renal function tests). Use of low therapeutic dose of aspirin is recommended.
The onset majority of potential interactions documented unspecified (67.2%) onset of action; based on Micromedex checker the time of the occurrence of interactions were not well established. pDDIs with possible rapid onset accounts 14% and with delayed onset had magnitude of 18.8%. If the clinical manifestation of the interaction may occur within 24 hours of after administering the potentially interacting drugs, it is considered having rapid onset whereas delayed; if it needs greater than 24 hours from the time of administration. Rapid onset requires immediate intervention but delayed more time for consideration of specific, practical options.
Our study also highlighted a significant association between pDDIs and age, sex and number of drugs. In our multivariate model, age of 70-74 years was associated with about two-fold increase in the adjusted odds of pDDIs, while female patients were 0.8 times less likely to develop PDDs. For patients 5 or 4 drugs and those of 5 and above drugs, the adjusted odds of pDDIs were 13 and 33 times as compared to that of other patients respectively. This supported by other studies which concluded that poly pharmacy is significant association with pDDIs.
Limitations of this Study
Quantitative determination of polypharmacy as the prescribing of 5 or more medications regardless of disease condition and the appropriateness of the prescribed medicines per diagnosis was not reviewed. Cross-sectional nature of the study designs my result for poor generalizability. The web-based or online multi-drug interaction checkers, Micromedex, used in this research study for the analysis of pDDIs were considered to have sufficient sensitivity and specificity towards identifying a potential drug interaction and the exact consequence of the interaction were not determined.
Conclusion
In conclusion, the present hospital-based study supports previous scientific evidence. Polypharmacy and pDDIs are higher in magnitude and might consequence significant health and economic burden. The findings have important implications in designing the mechanism for assessing polypharmacy and pDDIs. It will be better if future researchers conduct a follow-up study for actual consequence of drug interaction by determining serum concentration of the interacting drug.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Acknowledgement
None.
Competing Interest
None.
Ethics Approval
Wollo University health science college ethical review board approved this study. Approval letters obtained from the review board to precede the study.
References
- G. Kaur, Polypharmacy: The past, present and the future, J Adv Pharm Technol Res, 4(2013):224-5.
- N. Masnoon, S. Shakib, L. Kalisch-Ellett, G.E. Caughey, What is polypharmacy? A systematic review of definitions, BMC Geriatr, 17(2017):230.
- S. Shaojun, U. Klotz, Age-related changes in pharmacokinetics, Curr Drug Metab, 12(2011):601-10.
- A.A. Mangoni, S.H.D. Jackson, Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications, Br J Clin Pharmacol,
57(2004):6-14. - C. Hajat, E. Stein, The global burden of multiple chronic conditions: A narrative review, Prev Med Rep, 12(2018):284-293.
- M. Hermann, N. Carstens, L. Kvinge, A. Fjell, M. Wennersberg, et al. Polypharmacy and potential drug-drug interactions in home-dwelling older people-a cross-sectional study, J Multidiscip Healthc, 14(2021):589-597.
- E. Ramsdale, M. Mohamed, V. Yu, E. Otto, K. Juba, et al. Polypharmacy, potentially inappropriate medications, and drug-drug interactions in vulnerable older adults with advanced cancer initiating cancer treatment, Oncologist, 27(2022):e580-e588.
- N.J. Jackson, J.D. Isen, R. Khoddam, D. Irons, C. Tuvblad, et al. Potential drug-drug interactions among hospitalised elderly patients in Northern Sri Lanka, a lower middle-income country: A retrospective analysis, Drugs Real World Outcomes, 10(2023):83-95.
- F. Teka, G. Teklay, E. Ayalew, T. Teshome, Potential drug-drug interactions among elderly patients admitted to medical ward of ayder referral hospital, Northern Ethiopia: A cross sectional study, BMC Res Notes, 9(2016):431.
- M. Carpenter, H. Berry, A.L. Pelletier, Clinically relevant drug-drug interactions in primary care, Am Fam Physician, 99(2019):558-564.
Copyright: © 2023 Endalifer BL, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

