Research Article: Journal of Drug and Alcohol Research (2025) Volume 14, Issue 4
Eradication of Neurocysticercosis in South Africa Without Mass Drug Therapy
Lourdes de Fatima Ibanez Valdes1 and Humberto Foyaca Sibat2*2Department of Neurology, Nelson Mandela Academic Hospital, Walter Sisulu University, South Africa
Humberto Foyaca Sibat, Department of Neurology, Nelson Mandela Academic Hospital, Walter Sisulu University, South Africa, Email: humbertofoyacasibat@gmail.com
Received: 06-May-2024, Manuscript No. JDAR-25-165179; Editor assigned: 08-May-2024, Pre QC No. JDAR-25-165179 (PQ); Reviewed: 22-May-2024, QC No. JDAR-25-165179; Revised: 12-Aug-2025, Manuscript No. JDAR-25-165179 (R); Published: 19-Aug-2025, DOI: 10.4303/JDAR/236441
Abstract
Introduction: Taenia solium Taeniasis/Cysticercosis (TSTC) is a preventable foodborne, zoonotic, neglected tropical disorder predominantly seen in persons living or visiting low-and middle‐income endemic countries. Neurocysticercosis (NCC) is the consequence of invasion by the same cestode into the brain, optic nerves, or spinal cord. The cestode is identified as the larva form of the pig tapeworm Taenia solium (Ts).
Methods: We searched the literature, following the guidelines outlined in the PRISMA statement. From January 1985 to January 2025, the authors searched the scientific databases Scopus, Embassy, Medline, and PubMed Central using the following searches: “eradication of taeniosis/ cysticercosis” OR “eradication of NCC” OR “control of NCC” OR “control of taeniosis/cysticercosis “OR “mass drug therapy for NCC, OR “mass pig vaccination”.
Results: After screening the full‐text articles for relevance, 32 were included in the final review. However, no article was selected when we searched for the eradication of NCC without pig vaccination/ mass drug therapy.
Conclusions: No country worldwide has reported the eradication of active NCCs in this century. For more than ten years, nobody died in South Africa due to active NCC, and no dangerous presentations of NCC for life were identified. Only sporadic cases presenting calcified NCC still coming for medical care of secondary epilepsy.
Keywords
Eradication of NCC; Eradication of cysticercosis; Control of Taeniasis/Cysticercosi
Introduction
Taenia solium Taeniasis/Cysticercosis (TSTC) is a preventable foodborne, zoonotic, neglected tropical disorder predominately seen in persons living or visiting low and middle-income endemic countries, at the same time, Neurocysticercosis (NCC) is the consequence of invasion by the same cestode of the brain, optic nerves or the spinal cord which is identified as the larva form of the pig tapeworm Taenia solium (Ts). The most typical clinical features of this condition are Epilepsy (EP), Epileptic Seizures (ES) and headache, among other problems.
Pigs act as intermediate of cysticercosis while humans are definitive hosts. Taeniasis, i.e., intestinal infection with mature T. solium in the human host, occurs after ingesting undercooked measly pork meat infected with the larval stage (porcine cysticercosis). Cysticercosis in human beings occurs after humans ingest T. solium eggs or proglottids. NCC is the principal aetiology of secondary epilepsy in endemic areas [1–5]. ES and Ep are the most common symptoms of Cerebral Cysticercosis (CC). In the past, we performed more than a dozen epidemiological studies in rural areas around Mthatha, confirming that CC, also named Neurocysticercosis (NCC), is the primary aetiology of secondary epilepsy. Most ES and Ep respond well to first-line Antiepileptic Drugs (AED) and Antiseizure Medication (ASM) [6–15]. The most prescribe ASM is benzodiazepine, and the commonest used AED are valproic acid and carbamazepine [16–19]. Other aspects related to microglia and astrocyte expression at the centre of NI pathways have been investigated by our group, including the role of proinflammatory elements, such as chemokines and cytokines and upregulation of BBB disrupting proteinases in aspects of NCC [20–26]. In 2006, we also reported the clinical features and other aspects of Spinal Cord NCC (SCNCC) [27]. Recently, we highlighted the role played by pericytes in the pathogenesis of local neuroinflammation due to NCC, the healing process, and the prognosis of SCNCC [28].
The main goal of this review is to perform a bibliography investigation on the current situation of the eradication of NCC worldwide based on the reported information about it and to comment on the current situation of NCC in South Africa.
Materials and Methods
Search strategy
From January 1985 to January 2025, we investigated the databases Embassy, Medline, Scopus, and PubMed Central using the following searches: “eradication of taeniasis/ cysticercosis” OR “eradication of NCC” OR “control of NCC” OR “control of taeniasis/cysticercosis “OR “mass drug therapy for NCC” OR “mass pig vaccination.”
We searched the medical literature following the PRISMA guidelines. After removing duplicates, two reviewers (LDFIV and HFS) from each side screened titles and abstracts and evaluated the full texts of eligible articles based on the proposed inclusion criteria. Any disagreement between the reviewers involved in the literature search was resolved through discussion with all authors to reach a consensus.
Selection criteria
The following manuscripts were included in the systematic review:
Articles on Isaac syndrome, neuropathic pain, and Schwann cell disorder in ISA/NP, with detailed pathogenesis and/or drug therapy.
Exclusion criteria were as follows:
• Inaccessibility to full text.
• Articles with unclear pathogenesis.
• Lack of relevant clinicopathological data.
• Non-original studies (i.e., editorials, letters, conference proceeding, book chapters).
• Animal model studies.
• non-/Spanish/Portuguese/English studies.
The papers were thoroughly assessed, and duplicates were looked for.
Data extraction and quality assessment
All selected data were tabulated in an electronic Excel database. That information included pathogenesis, drug management, initial clinical presentation, evaluation of NP/IS after treatment, follow-up, and status at the latest evaluation. The studies’ quality was categorized as good, poor, fair, or reasonable, which agreed with the National Institutes of Health criteria. Two reviewers (LDFIV and HFS) independently evaluated the articles, and the discussion resolved disagreements.
Statistical analysis
The primary objective of this study was to evaluate whether the pathogenesis/drug management of DD differs significantly among different ways of therapies. Without a comprehensive reference for the total number of DD cases, the prevalence of DD responding to drug therapy with associated autonomic manifestations was searched through a thorough review.
Statistical analyses were performed using XLSTAT (add on for Microsoft Excel, version 2021.4.1, Addinsoft SARL) and RStudio. Variations in continuous variables were assessed using the Mann Whitney test. The Chi square test and Fisher’s exact were used to evaluate the association among categorical variables, as appropriate. We presented descriptive statistics for continuous variables as median (95% Confidence Interval (95% CI)). All situations were evaluated using the Kaplan-Meier method to identify relevant prognosticators. A model of multivariable Cox proportional hazards with a priori selection of covariates was used to check for independent prognostic effects.
To assess the therapy’s protective effect, we built a multivariable model that included only OMAS cases.
Results and Discussion
A total of 234 titles were selected from the search of medical literature. After removing duplicates and excluding records (N=127). One hundred seven relevant articles were examined. Twelve studies were unavailable for retrieving. After including five additional articles identified from citation searching (n=100), 63 were excluded for several reasons. A total of 32 records were identified from these searches. The resulting study titles were exported to Excel, and publications without including/excluding criteria duplicates were removed, leaving 32 unique titles. We screened all remaining unique full-text articles, abstracts, and titles for eligibility. Titles were typically excluded if they were unavailable in Spanish, Portuguese, or English or irrelevant to NCC/eradication. A total of 32 articles remained following this initial screening. The authors then screened these articles by abstract. After further review, abstracts were excluded if they were irrelevant to the topic, outdated, or unavailable in Spanish, Portuguese, or English. Thirty-four articles were for full-text review.
Finally, when we searched for eradication of NCC without pig vaccination and mass drug therapy, no article was identified
Series description and differences among groups
All the selected studies were relevant to the subject of this systematic review. None were randomized controlled trials or prospective studies; all the articles included were case reports and case series.
Median age was 29.5 (range 13-81) with significant differences between age groups (p<0.001). We did not find remarkable variations in gender (p=0.064), although females presenting NCC were noticeably more frequent and slightly more prevalent because most of the females remained at home while most male people moved out of Umtata/Mthatha to work in mine at the north of the country.
Brief comments on NCC in South Africa
Neurocysticercosis has been an endemic parasitic disease of South Africa localized almost strictly to Umtata/Mthatha and surrounding villages/locations (Former Transkei) in the province of Eastern Cape since the apartheid regimen from 1948 [10-12]. People living in this region needed to get a visa to pass the borders to visit other South African areas or to work in different kinds of mines in the north of the country, where they stayed from January to November and back home for a month in December, which happened for many decades. It has contributed to decreasing the spread of diseases all over the country. Therefore, only a few cases presenting NCC from other South African provinces have been reported since those times. The opening of a neurology service with high supporting facilities such as a well requipped clinical laboratory plus CT scan and MRI machines in a terminal in Mthatha to deliver direct neurological care to all rural communities around which has been another advantage of this region to afford the management of NCC for more than twentyeight years. Usually, the neurology services are in a big city of developing or developed countries.
Other advantageous regions in South Africa have access to clean water, good sanitation, and high education; pigs have no access to human faeces, as happened in our area (Figure 1).
Figure 1: Shows a picture of free-range pig eaten human faeces contam inated with eggs and proglottids of T. solium becoming an intermediary host of cysticercosis (porcine cysticercosis)
In another province, their inhabitants have better personal hygiene and proper meat inspection, and people do not consume infected pork meat (Figure 2).
Figure 2: Show a piece of pork meat with multiple cystic lesions from T. solium infection. Consumers said the flavour of that meat in sweet, and the meat is tender as well. If It’s freezing cysticercus died, if deep fried cooked the cysticercus also died but if it’s boiled (common way in deep rural areas) most of cysticercus will remains alive
In other provinces, the necessary conditions exist to prevent the progress of the life cycle of T. solium and the proliferation of taeniasis/cysticercosis. Therefore, human carriers from Umtata/Mthatha cannot disseminate the disease via porcine cysticercosis.
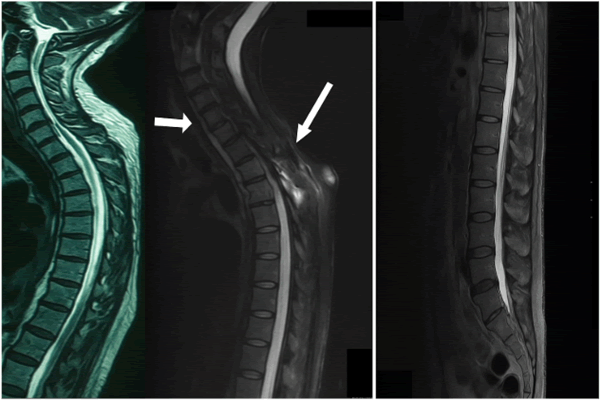
Soon after opening the neurology service in Mthatha in 1997, many clinical presentations of cysticercosis and NCC were quite commonly seen, including comorbidity of spinal cord neurocysticercosis and tuberculosis in HIV positive patients (Figure 3) [27].
Figure 3: Left: show an intramedullary cysticercus in the colloid stage at the cervical level. Center: Comorbidity of TB spine and intramedullary calcified NCC. Right: Shows a ring enhancing nodular lesion caused by intraspinal NCC
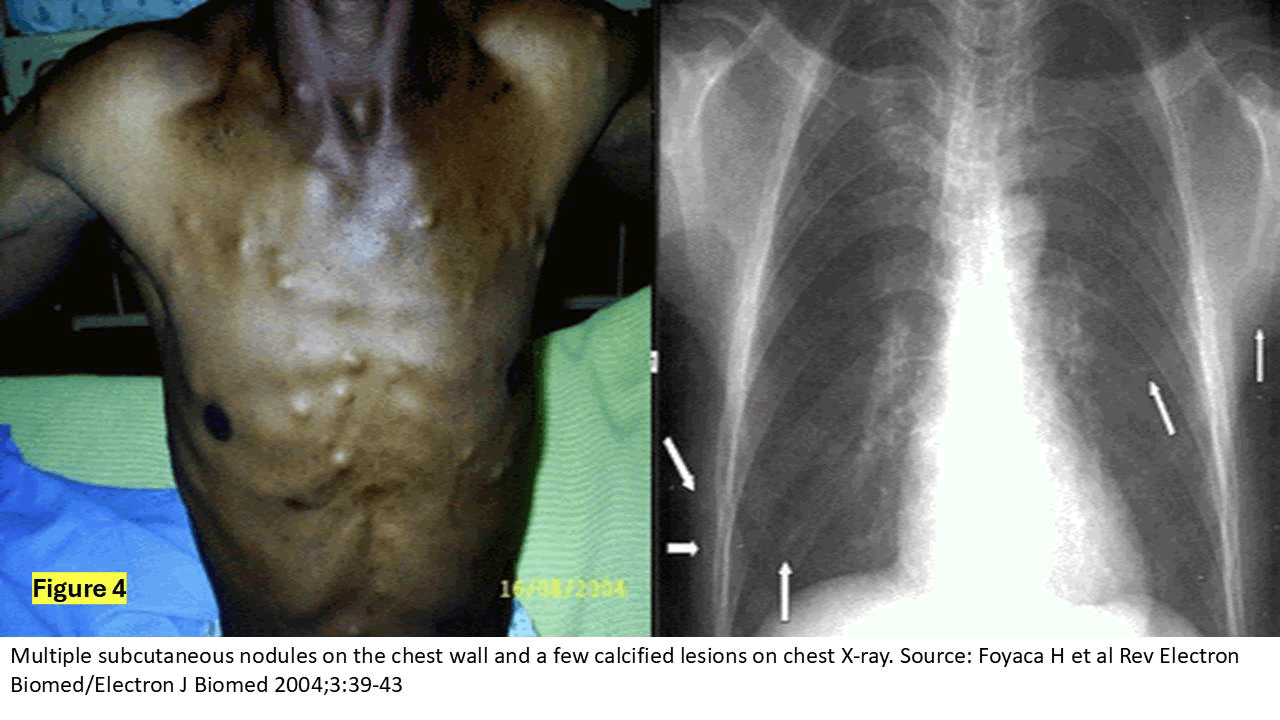
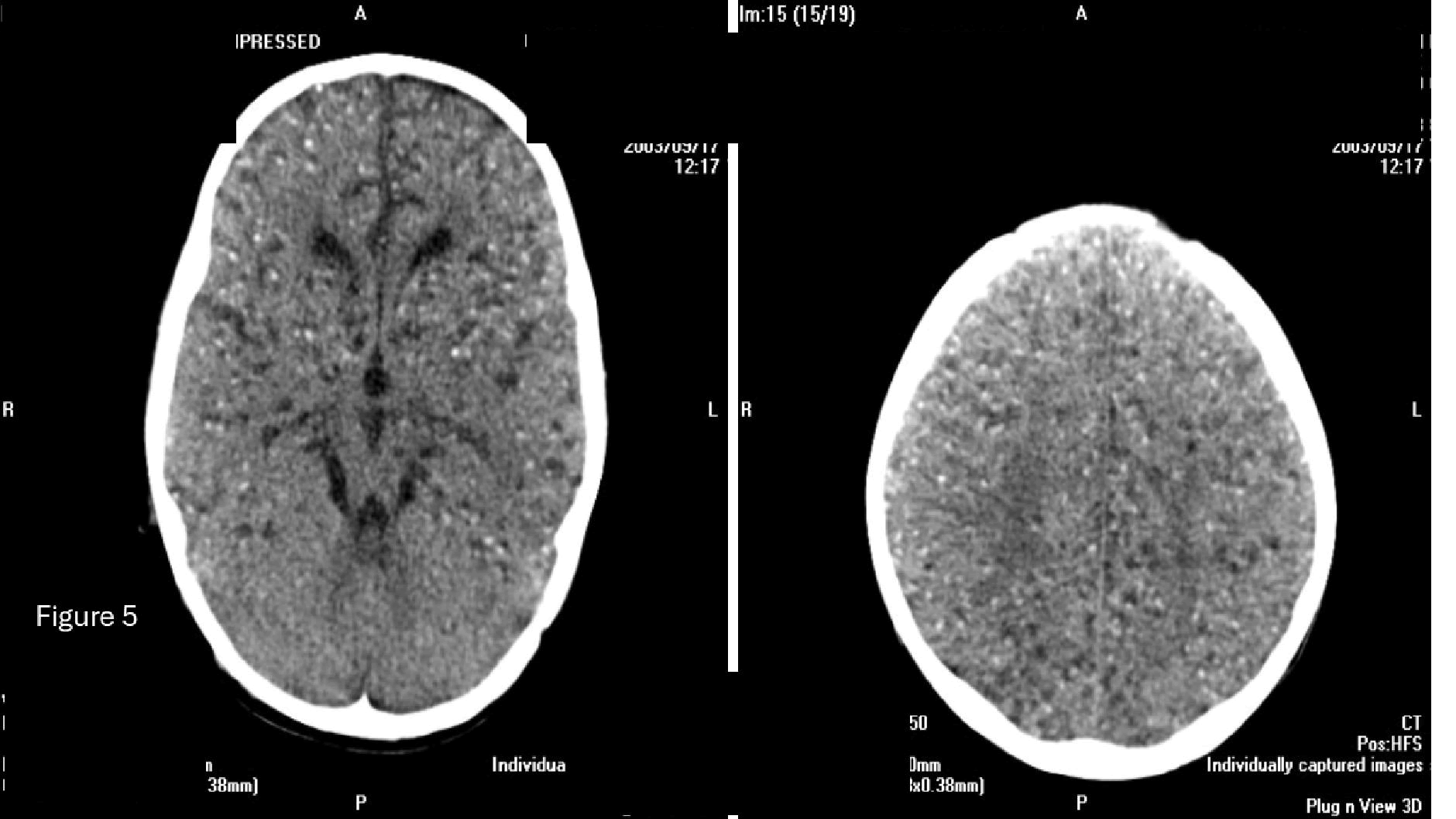
We’re also quite common to see comorbidity of NCC and HIV [28], comorbidity of NCC and Binswager’s disease [29], disseminated cysticercosis and massive NCC (Figures 4 and 5) [30].
Figure 4: It’s self-explanatory about disseminate cysticercosis with pul monary calcifications and multiple subcutaneous nodular calcifications on the chest
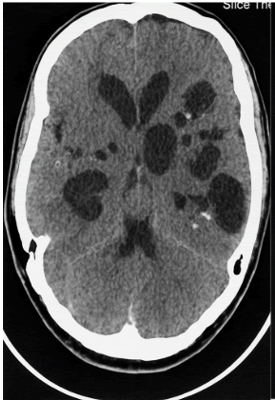
Figure 5: Axial view of CT scan of the brain showing massive NCC characterized by multiple and bilateral cystic lesions in colloid, nodular and calcified stages on both cerebral hemispheres and one active cysticercus on the left cerebellar hemisphere which less invade by cysticercus because of the hemodynamic characteristic of its blood supply
There are also cases presenting insula lobe NCC (Figure 6) [25,31], orbital cysticercosis, and cysticercosis of the extraocular muscles (Figure 7) [32,33].
Figure 6: Shows multiple active and calcified cysticercus at the anterior and middle aspect of the right insula lobe leading to insula lobe epilepsy
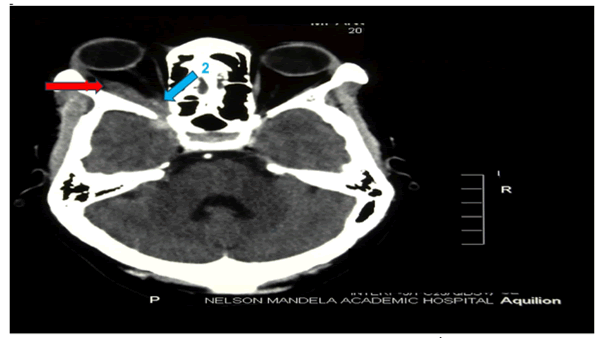
Figure 7: Axial view of the CT scan of the brain showing an intra orbital colloid stage of cysticercosis (2) affecting the lateral rectus and an associated local inflammatory reaction of its muscle fibres
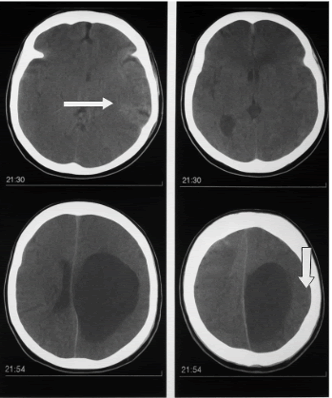
During those years, we also managed many patients presenting racemose/subarachnoid NCC (Figure 8) [14,16,35,36], Giant Intraparenchymal NCC cysts (Figure 9) [37], and intraventricular NCC (Figure 10) [34] among many other uncommon clinical manifestations of cysticercosis [38].
Figure 8: Axial view of CT scan of the brain with bilateral subarachnoid (racemose) NCC
Figure 9: Axial view of CT scan of the brain showing a calcified NCC on the frontal lobe and ipsilateral occipital active cysticercus with intracystic scolex and giant cyst in the parietal-occipital lobe
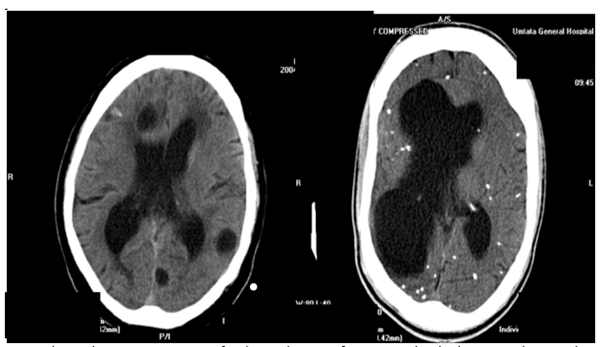
Figure 10: Axial view of the CT scan of the brain. On the right showing a bilateral obstructive hydrocephalus due to intraventricular NCC and bilateral cystic lesions at the colloid stage
During the implementation program for the eradication of NCC around Mthatha, we implemented many surveys door to door to determine the level of knowledge on NCC/ HIV/AIDS and the prevalence of epilepsy secondary to NCC and meeting to discuss health education, safe pig farming, latrine usage, food and personal hygiene, and how to recognise individuals with epilepsy. We trained all second-year medical students to speak Isi-Xhosa fluently in order to accomplish these goals. At the same time, they rotated through the Department of Community Medicine of the Walter Sisulu University (WSU) before they went to assess/interview the following locations/villages: Sidwadeni [2], Nkalukeni [13], Ngqwala [21], Ngangelizwe [22], Mdindweni [23], Mphumaze and Marahambeni [39], Makaula [40], Mngceleni [41] and many other endemic areas for NCC [42], as early as 2002, we start to investigate all aspects related with extra parenchymal presentations of NCC and performed including the clinical and neuroimmnological aspects of the intraventricular NCC in HIV patients [43].
In 2007 and 2008, to ensure receiving confident information and avoid bias, we encouraged the medical students to present their results in a scientific event in front of the highest university authorities of WSU as part of their assessment and final suitable qualification for the MBcHB II. In the following year, we reported on the accuracy of serological exams for the diagnosis of neurocysticercosis in outpatients with epileptic patients in the region of Lusikisiki, located about 127 km from Mthatha. We also correlated our laboratory findings with the information obtained from a brain CT scan. The first objective of this pilot study with 296 patients was to determine the prevalence of NCC in an epilepsy outpatient clinic for cysticercosis in an area of South Africa that is endemic to cysticercosis at the Nelson Mandela Academic Hospital. The second was to assess the accuracy of serological investigations in detecting NCC in that outpatient clinic and characterize sources of disagreement between serology and neuroimaging. The prevalence of NCC in Mthatha outpatients presenting epileptic seizures is like that observed in other countries where cysticercosis is prevalent [4].
Brief comments about the eradication of NCC in other countries
Between 1930 and 1960, four hundred fifty British soldiers returning from war in India were evaluated for epilepsy and other neurological disorders related to NCC, which is one of the most notable instances of the disease’s elimination in the United Kingdom [44]. The disease did not propagate to the country simply because the intermediary host (pigs) could not access the contaminated human faeces. Therefore, NCC disappeared.
Mexico has the longest history of investigating NCC and has made more efforts to eradicate the disease than Peru. However, Mexican investigators documented as early as 1966 that 2.8% of 884 autopsies made between 1947 and 1957 confirmed the diagnosis of NCC [45].
In 1985, Joubert and colleagues set the goal of eradicating NCC for the first time by administering praziquantel as a significant step towards eliminating this parasitic disease. However, to be effective, they considered it must take cognizance of reinfection, the allergic side effects caused by the dying parasites, and the probable situation of repeated courses of treatment to afford complete elimination of the parasite [46].
Eight years later, also in Mexico, Peter Schantz and collaborators documented that T. solium cysticercosis is an eradicable disease [47], and their arguments are summarized in Table 1.
Later, the same author, A Flisser, and other colleagues conducted a comprehensive study on the role of health education and the active participation of the population in eradicating NCC in Morelos, Mexico [48].
| Author (s) | Journal | Year | Reference | Proposal |
Documented |
|---|---|---|---|---|---|
| Joubert J, et al. | S Afr Med J | 1985 | 6;68(1):11-14 | Neurocysticercosis –a comprehensive approach to medical treatment |
Administration of praziquantel is a major step towards eradicating this pathological process. |
| Schantz PM, et al. | Bull Pan Am Health Organ | 1993 | 27(4):397–403 | Potential eradicability of taeniasis and cysticercosis |
a) Humans are the so definitive host (a condition called taeniasis) and are required to perpetua the lifecycle, b) Practical intervention was available in the form of mass chemotherapy for taeniasis with safe a efficacious drugs, c) Of exposure of domestic pigs, the on usual intermediary host, can be manage and d) The absence o wildlife reservoir. |
| Anonymous | MMWR Recomm Rep | 1993 | 31;42(RR-16):1-38 | Recommendations of the International task force for disease eradication |
|
| G Román, et al. | Bull World Health Organ | 2000 | 78(3):399-406 | A proposal to declare neurocysticercosis an international reportable disease |
The first step require to eradicate NCC is implement appropriate surveillance mechanisms under supervision of pub health authorities allowing the ration use of resources I eradication campaign. |
| Sotelo J | BMJ | 2003 | 8;326(7388):511-512 | Neurocysticercosis: Eradication of cysticercosis is an attainable goal |
Public education an sanitary measures the essential factors its disappearance which was accomplished long before the advent modern medical diagnostic neuroimaging and effective cysticidal education and pub awareness. |
| Engels D, et al | Acta Trop | 2003 | 87(1):177-182 | The control of human neurocysticercosis: Which way forward? |
Commitment of local and national authorities to control NCC needs to be convincingly solicit. |
| Román GC | Rev Neurol | 2003 | 1-15;36(1):71-74 | Neurocysticercosis: A public health perspective |
The aim of the would be to f target and optimise the available resources in eradication campaigns. |
| Lightowlers MW | Dev Biol (Basel) | 2004 | 119:361-368 | Vaccination for the prevention of cysticercosis |
T. solium has been identified as a disease and increase attention is being play on efforts to control transmission of the parasite. |
| Flisser A, et al. | Infect Immun | 2004 | 72(9):5292-5297 | Induction of protection against porcine cysticercosis by vaccination with recombinant oncosphere antigens |
Administration of tw recombinant Taenia solium oncosphere antigens, (TSOL18 a TSOL45âÂÃÂÂÂÂÃÂÂÂ1A as vaccin to prevent transmits of cysticercosis through pigs. |
| Pawlowski Z, et al. | Int J Parasitol | 2005 | 35(11-12):1221-1232 | Control of Taenia solium taeniasis/cys ticercosis: From research towards implementation |
More effective collaboration between medical and veterinary services is mandatory apart from better me inspection, promotion of health education, protection of pigs against infection, mo active diagnosis and treatment of human taeniasis, improved surveillance preparin and massive chemotherapeutic a sanitary intervention. |
| Willingham AL 3rd and Engels D. | Adv Parasitol | 2006 | 61:509-666 | Control of Taenia solium cysticercosis /taeniosis |
Authors consider the tools available for combating cysticercoid and suggest simple packages of interventions, utilizing existing services and structures in the endemic countries to provide appropriate and sustainable cont of the disease. |
| Garcia HH, et al. | J Neurol Sci | 2007 | 15;262(1-2):153-157 | Strategies for the elimination |
Development of a porcine vaccine agai cysticercosis and taeniasis/cys ticercosis and the cysticercosis have only been successful in temporarily disrupting transmission of the disease. |
| Flisser A and Correa D | PLoS Negl Trop Dis | 2010 | 4(12):e831 | Neurocystice rcosis may no longer be a public health problem in Mexico |
After the establish of a National Program for the Control of Taenia solium the general improvement of living conditions in Mexico increased remarkably which can explain the drastic reduction in the prevalence of NCC of the past decades although the parasite has not been eradicated |
| Lightowlers MW | Int J Parasitol | 2010 | 40(10):1183-1192 | Eradication of Taenia solium cysticercosis: A role for vaccination of pigs. |
The application of vaccine together with single treatment with oxfendazole achieved the complete elimination of transmission of the parasite by pigs involved in the field |
| Medina MT, et al. | Epilepsia | 2011 | 52(6):1177-1185. | Reduction in rate of epilepsy from neurocysticercosis by community interventions: The Salamá, Honduras study |
This populationâÂÃÂÂÂÂÃÂÂÂbas study evaluated the impact of an 8âÂÃÂÂÂÂÃÂÂÂyear public health and educational interment program in reducing symptomatic epilepsy in rural Salamá, Honduras. |
| Gilman RH, et al. | Pathog Glob Health | 2012 | 106(5):312–318 | Prevention and control of Taenia solium taeniasis/cysticercosi s in Peru |
Affected by geographical and climatic variations, different pig rearing systems, people’s attitudes towards medical and veterinary interventions, differed stages of development |
| Hélène Carabin and Aminata A Traoré | Curr Trop Med Rep | 2014 | 1(4):181-193 | Taenia solium taeniasis and cysticercosis control elimination through community based interventions |
Through wellâÂÃÂÂÂÂÃÂÂÂdesign solium taeniasis and communityâÂÃÂÂÂÂÃÂÂÂbased randomized control and trials that improve sanitation and pig management which more effective an sustainable than vaccination, human porcine mass treatment. |
| S Gabriël, et al. | Vet Parasitol | 2015 | 213(1-2):38-45 | Human migration and pig/pork import in the European Union: What are the implications for Taenia solium infections? |
HumanâÂÃÂÂÂÂÃÂÂÂtoâÂÃÂÂÂÂÃÂÂÂhuman transmission is the highest risk, prevention strategies should focus on the early detection and treatment of tapeworm carriers, a should be designed I concerted way, across the EU and across the different sectors. |
| Garcia HH, et al. | N Engl J Med | 2016 | 374(24):2335-2344. | Elimination of Taenia solium transmission in Northern Peru |
The disease is eradicable, but data attempts at regional elimination are lacki. We conducted a three phase control program in Tumbes, Peru, t determine whether regional elimination would be feasible. |
| World Health Organization | WHO | 2016 | Preventable epilepsy |
Taenia solium infect burdens economies societies and individuals, a ration for investment an action. |
|
| Carpio A, et al. | Expert Rev Neurother | 2018 | 18(4):289-301 | Neurocysticercosis: The good, the bad, and the missing |
Many tools for prevention and control of taeniasis/cysticercosis are available, but strategy to eradicate NC must be created with the involvement of all stakeholders. |
| Ngowi HA, et al. | PLoS One | 2016 | 14(6):e0217420 | Taenia solium taeniasis and cysticercosis literature in Tanzania provides research evidence justification for control: A systematic scoping review |
National elimination the parasite is the foundation for glob eradication. This w require that substance countryâÂÃÂÂÂÂÃÂÂÂlevel information is provide to all key stakeholder |
| CystiTeam Group for Epidemiology and Modelling of Taenia | 2016 | 26(3):1546 | The World Health Organization 2030 goals for Taenia solium: Insights and perspectives from transmission dynamics modelling |
Proposed a new modified Taenia solium transmission models which will support the achieve 2030 goals including socioâÂÃÂÂÂÂÃÂÂÂeconomic elements. |
|
| Men-Bao Qian, et al. | Adv Parasitol | 2020 | 110:289-317 | Control of taeniasis and cysticercosis in China |
The widespread implementation of deworming protocol and techniques for inspection, management and treatment of pigs a well as improved sewage management has contributed to the significant decrease taeniasis and cysticercoids in northern China. |
| Nsadha Z, et al. | Infect Dis Poverty | 2021 | 10(1):34 | Control trial of porcine cysticercosis in Uganda using a combination of the TSOL18 vaccination and oxfendazole |
This procedure has the potential to decrease the transmission of T. solium in Uganda another endemic countries. |
| Rimanpreet Kaur, et al. | Expert Review of Vaccines | 2021 | 20(11):1447-1458 | Vaccine for a neglected tropical disease Taenia solium cysticercosis: Fight for eradication against all odds. |
the total elimination NCC can be achieved good hygiene, mas importantly vaccinate of pigs or humans. |
| Dixon M | Adv Parasitol | 2021 | 112:133-217 | Taenia solium taeniasis/cysticercosi s: From parasite biology and immunology to diagnosis and control. |
CrossâÂÃÂÂÂÂÃÂÂÂsectoral interventions which target the parasite both the human and host provide the more effective approach for achieving control and ultimately eradication of NCC. |
| Nekrasova N, et al. | Med Glas (Zenica) | 2021 | 18(2):444-449 | Neurocysticercosis with symptomatic epilepsy manifestation |
With well-planned eradication program targeting all stages of Taenia solium life cycle, this zoonotic parasitic is potentially eradicable. |
|
Garcia HH, et al. |
JAMA Neurol |
2021 |
78(9):1045-1046 |
Neurocysticercosis as an eradicable cause of epilepsy: A plan and actions are needed |
Authors confirmed to interruption of T. solium transmission be transient if there not active efforts to maintain this state including a strict control of new migrant carrying T. solium infection. |
|
Del Bruto O |
Pathogens |
2022 |
20;11(10):1212 |
Human neurocysticercosis: An overview |
Efforts should be directed to eradicate the disease through implementation of control programs against all the steps. If the life cycle of T. solium, including carriers of the adult tapeworm, infected pigs, and eggs in the environment. |
|
Pineda-Reyes R and Clinton White A Jr |
Curr Opin Infect Dis |
2022 |
35(3):246-254 |
Neurocysticercosis: An update on diagnosis, treatment, and prevention. |
Field studies are demonstrating the feasibility of eradicate of NCC using a combination of mass chemotherapy for human tapeworms a vaccination/treatment of porcine cysticercoid. |
|
Hossain MS, et al. |
Parasit Vectors |
2023 |
24;16(1):380 |
Insights into the diagnosis, vaccines, and control of Taenia solium, a zoonotic, neglected parasite. |
Treatment of porcine cysticercosis, tapeworm carriers and prevention of disease transmission remain the principal. |
Table 1: Key literature on the control, elimination, and potential eradication of Taenia solium taeniasis/cysticercosis and neurocysticercosis.
Since 2000, scientists working in the NCC proposed that it should be declared an internationally reportable disease. Physicians or hospital administrators should report new cases to their health authorities [49] and from there to the highest international registering centre, which will contribute to an epidemiological intervention, support to interrupt the chain of transmission, to provide a better understanding of this problem and facilitate further action programmes for its eradication.
Table I summarises the author’s criteria for eradicating NCC [49].
Julio Sotelo from Mexico documented the basic mechanism for eradicating NCC based on its development and outcome in Germany and his knowledge of its origin history. He also noted the advantages of neuroimaging studies (CT scan, MRI) and the advent of effective antiparasitic medication (albendazole and praziquantel) [50].
Engels and collaborators also considered NCC a potentially eradicable disease but did not find evidence to sustain that it is feasible and recommendable to envisage this within a reasonable time frame. However, they concluded that local and national authorities’ commitment to control NCC must be convincingly solicited, and, as for most zoonotic diseases, an interdisciplinary approach is essential [51].
Also, in Mexico together with Cameroon, two recombinant Taenia solium oncosphere antigens (TSOL18 and TSOL451A as vaccines) were administered to prevent transmission of cysticercosis through pigs, obtaining the highest level of protection against T. solium infection in pigs by vaccination. These two vaccines are highly effective and can support the control of cysticercosis and, potentially, the eradication of human NCC [52].
But the following year, additional researchers took into account the biology of T. solium, its reservoirs and modes of transmission, and the possibility of completely eliminating Taenia solium taeniasis and cysticercosis worldwide. However, they finally concluded that global eradication of T. solium infection is unlikely because low sanitation and health education levels amongst endemic populations, ineffective health services infrastructure and inadequate socioeconomic development persist [53,54].
Pawlowski et al., considering the biology of transmission and reservoirs of cysticercosis, documented that global eradication of Taenia solium taeniasis and cysticercosis is feasible but still unlikely soon due to ineffective health services infrastructure, low levels of sanitation and health education amongst endemic populations, and inadequate socioeconomic development in these endemic areas. They concluded that to implement control measures in endemic regions of cysticercosis, more effective collaboration between medical and veterinary services is mandatory apart from better meat inspection, promotion of health education, protection of pigs against infection, more active diagnosis and treatment of human taeniasis, improved surveillance preparing and massive chemotherapeutic and sanitary interventions [53,54].
Garcia and collaborators reported that mass chemotherapy effectively decreased infection pressure in a hyperendemic area of Peru, although the effect reached after therapy was too small. Therefore, it did not attain the goal of eliminating transmission [55].
Despite being deemed eradicable and theoretically simple to control, NCC is still ignored in the majority of endemic nations because of a lack of awareness, information, proper diagnostic and management capabilities, and prevention and control methods. When larval cysts form in the brain, human neurocysticercosis happens [56].
Several proposals have been implemented to eradicate NCC with active participation, such as community health education, mass chemotherapy of porcine cysticercosis, changing domestic pig raising farming, and selective detection and treatment of taeniasis. The development of a porcine vaccine against cysticercosis and ongoing progress in the diagnosis of taeniasis and cysticercosis have only successfully temporarily disrupted the transmission of the disease. Therefore, controlled data on the efficacy and acceptability of the different interventions is prompt needed to provide a baseline schematic for the eradication of NCC from each endemic scenario [57].
After the establishment of a National Program for the Control of Taenia solium, the general improvement of living conditions in Mexico remarkably increased, which can explain the drastic reduction in the prevalence of NCC over the past decades, including better socioeconomic and health conditions regarding risk factors for NCC, a steep increment in household facilities: Domiciles with piped water and proper sewage, remarkable electrification of the country, the increment of toilets facilities plus the decreased rate of population growth, fecundity, mortality, and the number of people in households. On top of that, there is an increase in the number of schooling years, increased income per capita, and improved infrastructure, leading to better communication among all communities and better access to health and education personnel. However, this viewpoint does not imply that the parasite has been eradicated [58].
Lightower’s documented that the vaccine application and a single treatment of pigs with oxfendazole eliminated the parasite transmission by pigs involved in the field trial [59]. However, sustainable reports about permanent eradication of porcine cysticercosis have not been documented later.
Peru is the country where more attempts to eradicate NCC have been unsuccessful. Some Peruvian investigators have considered that this is due to geographical and climatic variations, different pig rearing systems, people’s attitudes towards medical and veterinary interventions, various stages of development, social determinants, and a lack of close interaction between medical and veterinary services involved in the eradication program [60].
In 2012, Fleury et al. established that NCC is still a prevalent public health problem in Mexico and recommended further measures to control and eventually eradicate T. solium [61].
The magnitude of NCC in some Western European countries from 1970 to 2011 was determined by Del Brutto in 2012. The most affected countries were Portugal (n=384), Spain (n=228), France (n=80), The United Kingdom (n=26), and Italy (n=21), suspecting that the prevalence of NCC in Western Europe may be on the rise. While other authors reported similar/different findings in Europe and other countries before and after this publication [54, 62-79].
Carabin and Traoré reported that T. solium was identified as potentially eradicable by the International Task Force for Disease Eradication in 1992 and established that eradication of NCC is feasible through community based interventions to support the effect and cost effectiveness of alternative control strategies for NCC [80].
Some authors considered that the increase in the number of detected patients with NCC is due to human migration and the movement of pigs/pork. However, they concluded that entering a tapeworm carrier into the EU is more likely than importing infected pork. As we summarized in Table 1, these investigators concluded that human-to-human transmission is the highest risk. Therefore, prevention strategies must focus on the early detection and management of tapeworm carriers across the EU [81].
In 2017, other authors [76] found reported cases of T. solium infection in France, Italy, Spain, Slovenia, Denmark, Portugal and the UK. Cases presenting NCC were reported in all Western European countries except for Iceland, which was more prevalent in Portugal and Spain. Most cases of NCC acquired the infection outside Western Europe. Cases of T. solium in pigs were found in Portugal and Austria. Spain, Germany, and Slovenia have been informed about pigs affected by cysticercosis. Unfortunately, the current situation regarding sustainable action programs for eradicating NCC in these countries remains unknown.
Many tools for preventing and controlling taeniasis/ cysticercosis were reachable, but the authors considered that programmes to control/eradicate NCC must be created with the participation of all stakeholders [82].
Table condenses the documentation from Ngowi et al. on eradicating cysticercosis in Tanzania. They studied over f ifty publications about this issue and concluded that three rounds of annual therapy of school age children with praziquantel significantly decreased the prevalence of taeniasis and porcine cysticercosis [83].
The CystiTeam Group for Epidemiology and Modelling of Taenia solium Taeniasis/Cysticercosis proposed a new modified Taenia solium transmission model that will support the achievable 2030 goals, including socioeconomic elements, adequate understanding of underlying biological processes and consideration of spatial dynamics [84].
In China, some authors have found that administering pumpkin seeds and areca nuts has improved the control of taeniasis, while praziquantel and albendazole are prescribed against cysticercosis with good efficacy and low side effects. They propose extending this therapy to highly endemic areas in western China to eliminate taeniasis and cysticercosis nationally [85].
Kaur et al. established that epilepsy caused by T. solium is a preventable condition, and the total eradication of NCC can be achieved by mass therapy, good hygiene, and, most importantly, vaccination of pigs or humans [86].
In order to achieve the objectives of the WHO neglected tropical diseases roadmap for 2021–2030, which was approved in November 2020, Dixon and colleagues have shown that the most effective methods for controlling and eventually eliminating NCC are cross-sectoral interventions that target the parasite in both human and pig hosts [87].
This zoonotic parasitic is potentially eradicable with well planned eradication programs targeting all stages of Taenia solium life cycle [88].
In 2021, another investigator administered the TSOL18 vaccine and oxfendazole to a group of selected pigs and concluded that the procedure could potentially decrease the transmission of T. solium in Uganda and other endemic countries [89].
Based on the current epidemiological conditions, some authors have considered that NCCs will not be controlled in a short period of time term; instead, their incidence will likely increase along with inequality, poverty, and related socioeconomic problems [90].
From 2003 to 2013, some authors conducted a comprehensive elimination demonstration program in Tumbes (on Peru’s Northern Coast) with the goal of proving that T. solium transmission could be stopped regionally. They showed that in a subset of villages, the interruption of transmission continued for a year after the intervention ended in a sizable percentage of intervened villages. However, they could not sustain those achievements because they could not control the migration from other endemic areas. Therefore, the scientists found that if there are no active attempts to maintain this situation, such as careful management of migrant carriers of T. solium infection, the interruption of T. solium transmission may be temporary. Lastly, these authors think that the only way to eradicate NCC is to first achieve focal elimination, then expand these areas to achieve widespread elimination and ultimately eradication, rather than waiting years for development to reach the impoverished, rural areas that are primarily affected by this eradicable disease [91].
In some Caribbean countries like Cuba, NCC never was an endemic parasitic disease. Therefore, it wasn’t eradicated because it never was a prevalent public health problem apart from a few cases reported. It is also vital to ensure that T. solium remains absent from Cuba [92], field investigations show that mass chemotherapy for human tapeworms and a combination of pig cysticercosis vaccine and treatment can effectively eradicate NCC [93]. However, several writers have shown that treating porcine cysticercosis, tapeworm carriers, and prevention of disease transmission remain the principal goals of interrupting the zoonotic cycle of T. solium in endemic countries. Some authors expressed that “ it is still far from being achieved despite eradication of TSTC appearing possible in principle” [94].
As part of the program to eradicate NCC, we conducted other investigations over those years to clarify the immunopathogenesis of NCC in our region. We studied other comorbidities, the role of oxidative stress, programmed cell death, regulated cell death, ferroPANoptosis, Cuproferropanoptosis, and the role of supporting cells in NCC, and those results are fully available on the Internet [95-104].
Since 2013, we documented that Homo Ergaster is represented by fossils such as “Nariokotome Boy” he was born in sub-Saharan Africa. He was probably the first human infected by T. solium from contaminated lions and hyenas many centuries before pigs became an intermediate host. Now it’s our honour to announce that the mortality rate caused by NCC is cero in this part of the world, and the disease has been controlled thanks to the collaboration of many institutions and organizations, including the 2004 Cysticercosis Working Group for Eastern and Southern Africa’s awareness workshop and 2011 general assembly which made a significant contribution to the Mthatha eradication program of NCC (Figure 11).
Figure 11: On the right side: Participants in the Cysticercosis Working Group for Eastern and Southern Africa (CWGESA) Cysticercosis/ Taeniosis Awareness Training Workshop held in University of Transkei in Mthatha on the 7-11 June 2004 with the participation of eleven delegates from different African countries. Among the participants were Dr B Gqwana The MEC Health in Easter Cape Province, Prof L Mazwai, The Dean of Faculty of Health Sciences, Prof A Awotedu HOD of Internal Medicine and the most relevant investigators of this field participating were Prof T Nash, Prof Lee Willingham, Prof Tammy Krecek, Prof H Foyaca, Prof Linda Cowan and Prof Helene Carabin. Here, the road walk program for eradication of NCC and the creation of the International Center for NCC in Mthatha was approved. On the left side of the picture the participants of the 7th CWGES General Assembly held in University of Walter Sisulu, Mthatha, South Africa on 20-22 July 2011 where the progress of the program for eradication of NCC was assessed with the participation of Prof Lee Willingham 3rd, Prof Samson Mukaratirwa, Prof Humberto Foyaca Sibat, Prof Helen A Ngowi, Prof MN Lightowlers and many others
Source: Cysticercosis Working Group for Eastern & Southern Africa 7th CWGESA General Assembly Meeting Mthatha Health Resource Centre Waltr Sisulu University, South Africa
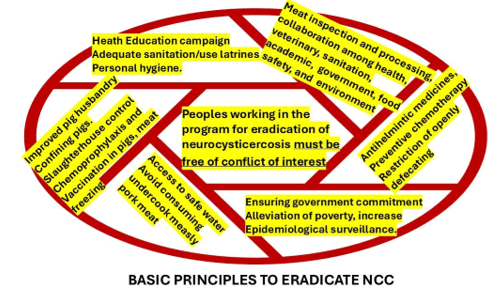
The most important rules to eradicate are summarized in Figure 12. But we want to emphasise that we didn’t vaccine the pigs or provide them antiparasitic medications, and we did not implement mass drug therapy with Praziquantel and Albendazole to our population because we did not know if any patient presented intraocular/orbital cysticercosis. We want to avoid iatrogenic damage. We included these rules in the list to eradicate NCC and to be free of conflict of interest because we are sure that any person or group receiving benefits from the fight against NCC obviously will not be interested in solving this problem.
Figure 12: Shows the most important rules that must be followed to eradicate NCC worldwide. One of the highlighted rules is related to peoples involved in the process of elimination of NCC whom should free of any conflict of interest including receiving money, travelling the world or getting any personal benefit, they should follow only professional rules such as special dedication to the program, commitment and hight level of responsibility to reach the crucial role of eliminate NCC worldwide
Conclusion
Over the past ten years, all disseminated, massive, fatal and extra parenchymal NCC presentations never happened again, and nobody died due to NCC. On the other hand, only sporadic new epileptic patients with calcified NCC are seen in our hospital. Therefore, until proven otherwise, NCC has been eradicated in Mthatha. As far as we know, it is the first report on eradicating NCC in Africa.
Author Contributions
Both investigators have read and agreed to the published version of the manuscript.
Conflict of Interest Statement
The authors declare they have no conflicts of interest.
Funding Information
The authors received no funds to perform the present research.
Ethics Statement
The study was conducted using the principles of the Helsinki Declaration, the Italian and US privacy and sensitive data laws, and the internal regulations for retrospective studies of the Otolaryngology Section at Padova University and Brescia University.
Informed Consent Statement
We obtained the informed consent from the case involved in the study.
Data Availability Statement
The corresponding author will make the raw data supporting this article’s conclusions available upon request.
Acknowledgments
The authors thank Prof Thozama Dubula, Head of Department on Internal Medicine and Therapeutic for his unconditional support in the management of this patient.
References
- H. FoyacaâSibat, L. Ibañez Valdés, Pseudo seizures and epilepsy in neurocysticercosis, Electron J Biomed, 2(2003):20â29.
- H. FoyacaâSibat, A.R. Del Rio, L.F. IbañezâValdés, A. Awotedu, Neuroepidemiological survey for epilepsy and knowledge about neurocysticercosis at Sidwadweni location, South Africa, Electron J Biomed, 2(2004):40â48.
- H. FoyacaâSibat, L.F. IbañezâValdés. Insular neurocysticercosis: Our finding and review of the medical literature, Internet J Neurol, 5(2006).
- H. FoyacaâSibat, L.D. Cowan, H. Carabin, G. Serrano Ocana, R.C. Krecek, et al. Accuracy of serological exam for the diagnosis of neurocysticercosis in outpatients with epilepsy, Eastern Cape Province, South Africa, PLoS Negl Trop Dis, 3(2009):1â7.
- H. FoyacaâSibat, L. Ibañez Valdés, J. MoreâRodriguez, Parasitic zoonoses of the brain: Another challenger?, Int J Neurol, 12(2009).
- H. Carabin, R.C. Krecek, L.D. Cowan, L. Michael, H. FoyacaâSibat, et al. Estimation of the monetary burden of Taenia solium cysticercosis in the Eastern Cape, South Africa, Trop Med Int Health, 11(2006):906-916.
[Crossref] [Google Scholar] [PubMed]
- H. FoyacaâSibat, L.F. IbañezâValdés. Treatment of epilepsy secondary to neurocysticercosis, 2011.
- H. FoyacaâSibat, Epilepsy secondary to parasitic zoonoses of the brain, in: Novel Aspects on Epilepsy, H. FoyacaâSibat (Ed.), InTech, 2011.
- H. FoyacaâSibat, M. SalazarâCampos, L. IbañezâValdés, Cysticercosis of the extraocular muscles: Our experience and review of the medical literature, Internet J Neurol, 14(2012).
- H. FoyacaâSibat, L.F. IbañezâValdés, Uncommon clinical manifestations of cysticercosis, in: Novel Aspects on Cysticercosis and Neurocysticercosis, H. FoyacaâSibat (Ed.), InTech, 2013.
- H. Foyaca Sibat, L.F. Ibañez Valdés, What is a low frequency of the disseminated cysticercosis suggests that neurocysticercosis is going to disappear?, Novel Aspects on Cysticercosis and Neurocysticercosis, InTech, 2013.
- H. Foyaca Sibat, M.C. Salazar Campos, L.F. Ibañez Valdés, Orbital cysticercosis: A challenge for neurologists, ophthalmologists, neuro-ophthalmologists, and general practitioners, Novel Aspects on Cysticercosis and Neurocysticercosis, InTech, 2013.
- Del Rio-Romero, H. Foyaca-Sibat, L. Ibanez-Valdes, E. Vega-Novoa, Prevalence of epilepsy and general knowledge about neurocysticercosis at Nkalukeni Village, South Africa, Internet J Neurol, 3(2004):2.
- H. Foyaca Sibat, L.F. Ibañez Valdés, Subarachnoid cysticercosis and ischemic stroke in epileptic patients, Seizures, InTechOpen, 2018.
- Noormahomed EV, Nhancupe N, Mufume J, Schooley RT, Foyaca-Sibat H, et al. Neurocysticercosis in epileptic children: An overlooked condition in Mozambique, challenges in diagnosis, management and research priorities, EC Microbiol, 17(2021):5.
- H. Foyaca Sibat, Neurocysticercosis, epilepsy, COVID-19 and a novel hypothesis: Case series and systematic review, Clin Schizophr Relat Psychoses, 15S(2021).
- H. Foyaca Sibat, Neurocysticercosis, epilepsy, COVID-19 and a novel hypothesis: Case series and systematic review, Clin Schizophr Relat Psychoses, 15S(2021).
- H. Foyaca Sibat, Comorbidity of neurocysticercosis, HIV, cerebellar atrophy and SARS-CoV-2: Case report and systematic review, Clin Schizophr Relat Psychoses, 15S(2021).
- L.F. Ibañez Valdés, H. Foyaca Sibat, Psychogenic nonepileptic seizures in patients living with neurocysticercosis, Seizures, 2018.
- L.F. Ibañez Valdés, H. Foyaca Sibat, Psychogenic nonepileptic seizures in patients living with neurocysticercosis, Seizures, 2018.
- H. FoyacaâSibat, A. Del Rio, L. IbanezâValdes, E. Vega, A neuroepidemiological survey for epilepsy and knowledge about neurocysticercosis at Ngqwala location, South Africa, Internet J Neurol, 3(2004):2.
- H. FoyacaâSibat, D.R. Romero, L. Ibañez Valdés, Prevalence of epilepsy and general knowledge about neurocysticercosis at Ngangelizwe location, South Africa, Internet J Neurol, 4(2005):1.
- Del Rio, H. FoyacaâSibat, L. IbañezâValdés, Epidemiological survey about socioâeconomic characteristics of Mpindweni location, South Africa, Internet J Neurol, 4(2005):2.
- L.F. Ibañez Valdés, H. FoyacaâSibat, Meningeal lymphatic vessels and glymphatic system in neurocysticercosis: A systematic review and novel hypotheses, Clin Schizophr Relat Psychoses, 17(2023).
- H. FoyacaâSibat, L.F. IbañezâValdés, Insular neurocysticercosis: Our findings and review of the medical literature, Internet J Neurol, 5(2006):2.
- H. FoyacaâSibat, L. Ibañez Valdés, Coâmorbidity of spinal cord neurocysticercosis and tuberculosis in a HIVâpositive patient, Internet J Neurol, 7(2006):5–10.
- H. FoyacaâSibat, L.F. IbañezâValdés, Neurocysticercosis in HIVâpositive patients, Internet J Infect Dis, 2(2003):15-23.
- H. Foyaca Sibat, L.F. IbañezâValdés, Vascular dementia type Binswanger’s disease with active neurocysticercosis, Rev Electron Biomed/Electron J Biomed, 1(2003):32-42.
- H. FoyacaâSibat, L.F. IbañezâValdés, Disseminated cysticercosis with cardiac involvement, Internet J Neurol, 7(2007):6–11.
- H. FoyacaâSibat, L.F. IbañezâValdés, Clinical features of epilepsy secondary to neurocysticercosis at the insular lobe, in: H. FoyacaâSibat (Ed.), Novel Aspects on Epilepsy, InTech, 2011.
- H. Foyaca-Sibat, M. Salazar-Campos, L. Ibañez-Valdés, Cysticercosis of the extraocular muscles. Our experience and review of the medical literature, Internet J Neurol, 14(2012).
- HF. Sibat, MC. Campos, LD. Valdés, Orbital Cisticercosis. A challenger for neurologists, ophthalmologists, neuro-opthalmologists, and general practitioners. InNovel Aspects on Cysticercosis and Neurocysticercosis, IntechOpen, 2013.
- H. FoyacaâSibat, L. IbañezâValdés, Intraventricular Neurocysticercosis in HIV Positive Patients, Internet J Neurol, 2(2002).
- H. Foyaca-Sibat, IV. LdeF, J. Moré-Rodríguez, Parasitic zoonoses of the brain: Another challenger, Internet J Neurol, 2(2010):9-14.
- H. Foyaca-Sibat, Racemose Neurocysticercosis Long COVID and brainstem dysfunction: A case report and systematic review, Clin Schizophr Relat Psychoses, 2021.
- Foyaca-Sibat H, LdeF IV, Occipital lobe syndrome due to giant intraparenchymal neurocysticercosis, Internet J Neurol, 5(2006).
- HF. Sibat, LD. Valdés, Uncommon clinical manifestations of cysticercosis, InNovel Aspects on Cysticercosis and Neurocysticercosis, IntechOpen, 2013.
- H. Foyaca-Sibat, RI. Del Rio, Epilepsy, Neurocysticercosis and, Poverty at Mphumaze and Marhambeni Locations, in South Africa, Internet J Neurol, 7(2007):8-14.
- Del Rio RA, Foyaca-Sibat H, Ibanez-Valdes L, Neuroepidemiological survey for epilepsy, knowledge about epilepsy, neurocysticercosis and HIV/AIDS at the Makaula Village in South Africa, Internet J Neurol, 7(2007).
- AI. Del RioâRomero, H. FoyacaâSibat, IbanezâValdes, Neuroepidemiology findings as contributors for epilepsy due to neurocysticercosis at mngceleni location, South Africa, Internet J Neurol, 9(2008):33-40.
- H. Foyaca-Sibat, AI. Del Rio-Romero, Prevalence of epilepsy in an endemic area for neurocysticercosis in South Africa, Internet J Neurol, 9(2008):8-18.
- H. Foyaca-Sibat, L. Ibanez-Valdes, Neurocysticercosis in HIV-positive patients. The Internet J Neurol, 2(2003):15-23.
- HB. Dixon, FM. Lipscomb, Cysticercosis: An analysis and follow-up of 450 cases, (1961)
- SR. Macias, J. Hernandez Peniche, Cerebral cysticercosis: Clinical, radiological and laboratory diagnosis, prognosis, Prensa Med Mex, 31(1966):147-155.
- J. Joubert, MJ. Joubert, CM. Lombaard, Neurocysticercosis: A comprehensive approach to medical treatment, S Afr Med J, 68(1985):11-14.
[Google Scholar] [PubMed]
- P. M. Schantz, M. Cruz, E. Sarti, Z. Pawlowski, Potential eradicability of taeniasis and cysticercosis, Bull Pan Am Health Organ, 27(1993):397–403. [Crossref]
[Google Scholar] [PubMed]
- E. Sarti, A. Flisser, P. M. Schantz, M. Gleizer, M. Loya, et al., Development and evaluation of a health education intervention against Taenia solium in a rural community in Mexico, Am J Trop Med Hyg, 56(1997):127–132.
[Crossref] [Google Scholar] [PubMed]
- G. Román, J. Sotelo, O. Del Brutto, A. Flisser, M. Dumas, et al. A proposal to declare neurocysticercosis an international reportable disease, Bull World Health Organ, 78(2000): 399–406.
[Google Scholar] [PubMed]
- J. Sotelo, Neurocysticercosis: eradication of cysticercosis is an attainable goal, BMJ, 326(2003):511–512.
[Crossref] [Google Scholar] [PubMed]
- D. Engels, C. Urbani, A. Belotto, F. Meslin, L. Savioli, The control of human (neuro)cysticercosis: Which way forward?, Acta Trop, 87(2003):177–182.
[Crossref] [Google Scholar] [PubMed]
- Flisser, C. G. Gauci, A. Zoli, J. MartinezâOcaña, A. GarzaâRodriguez, et al. Induction of protection against porcine cysticercosis by vaccination with recombinant oncosphere antigens, Infect Immun, 72(2004):5292–5297.
[Crossref] [Google Scholar] [PubMed]
- Z. Pawlowski, J. Allan, E. Sarti, Control of Taenia solium taeniasis/cysticercosis: from research towards implementation, Int J Parasitol, 35(2005):1221–1232.
[Crossref] [Google Scholar] [PubMed]
- Pondja, L. Neves, J. Mlangwa, S. Afonso, J. Fafetine, et al. Prevalence and risk factors of porcine cysticercosis in Angónia District, Mozambique, PLoS Negl Trop Dis, 4(2010):e594.
[Crossref] [Google Scholar] [PubMed]
- H. H. Garcia, A. E. Gonzalez, R. H. Gilman, L. H. Moulton, M. Verastegui, et al. Combined human and porcine mass chemotherapy for the control of T. solium, Am J Trop Med Hyg, 74(2006):850–855.
[Google Scholar] [PubMed]
- Willingham III, D. Engels. Control of Taenia solium cysticercosis/taeniosis, Adv Parasitol, 61(2006):509–566.
[Crossref] [Google Scholar] [PubMed]
- H. H. García, A. E. González, O. H. Del Brutto, V. C. W. Tsang, F. Llanos-Zavalaga, et al. Strategies for the elimination of taeniasis/cysticercosis, J Neurol Sci, 262(2007):153–157.
[Crossref] [Google Scholar] [PubMed]
- Flisser, D. Correa, Neurocysticercosis May No Longer Be a Public Health Problem in Mexico, PLoS Negl Trop Dis, 4(2010):e831.
[Crossref] [Google Scholar] [PubMed]
- M. W. Lightowlers, Eradication of Taenia solium cysticercosis: A role for vaccination of pigs, Int J Parasitol, 40(2010):1183–1192.
[Crossref] [Google Scholar] [PubMed]
- R. H. Gilman, A. E. González, F. Llanos-Zavalaga, V. C. W. Tsang, H. H. García, Prevention and control of Taenia solium taeniasis/cysticercosis in Peru, Pathog Glob Health, 106(2012):312–318.
[Crossref] [Google Scholar] [PubMed]
- A. Fleury, E. Sciutto, C. Larralde, Neurocysticercosis is still prevalent in Mexico, Salud Publica Mex, 54(2012):632–636.
[Crossref] [Google Scholar] [PubMed]
- O. H. Del Brutto, Neurocysticercosis in Western Europe: A re-emerging disease?, Acta Neurol Belg, 112(2012):335–343.
[Crossref] [Google Scholar] [PubMed]
- R. Rodríguez-Canul, A. Fraser, J. C. Allan, J. L. Domínguez-Alpizar, F. Argaez-Rodriguez, et al. Epidemiological study of Taenia solium taeniasis/cysticercosis in a rural village in Yucatan state, Mexico, Ann Trop Med Parasitol, 93(1999):57–67.
[Crossref] [Google Scholar] [PubMed]
- D. K. Pal, A. Carpio, J. W. Sander, Neurocysticercosis and epilepsy in developing countries, J Neurol Neurosurg Psychiatry, 68(2000):137–143.
[Crossref] [Google Scholar] [PubMed]
- O. H. Del Brutto, R. Santibánez, L. Idrovo, S. Rodríguez, E. Díaz-Calderón, et al. Epilepsy and neurocysticercosis in Atahualpa: A door-to-door survey in rural coastal Ecuador, Epilepsia, 46(2005):583–587.
[Crossref] [Google Scholar] [PubMed]
- L. Willingham III, H. W. Wu, J. Conlan, F. Satrija, Combating Taenia solium cysticercosis in Southeast Asia: an opportunity for improving human health and livestock production, Adv Parasitol, 72(2010):235–266.
[Crossref] [Google Scholar] [PubMed]
- E. Leshem, I. Kliers, M. Bakon, T. Zucker, I. Potasman, et al. Neurocysticercosis in Israel, Harefuah, 149(2010):576–579.
- M. T. Medina, R. L. Aguilar-Estrada, A. Alvarez, R. M. Durón, et al. Reduction in rate of epilepsy from neurocysticercosis by community interventions: The Salamá, Honduras study, Epilepsia, 52(2011):1177–1185.
[Crossref] [Google Scholar] [PubMed]
- S. Winkler. Neurocysticercosis in sub-Saharan Africa: A review of prevalence, clinical characteristics, diagnosis, and management, Pathog Glob Health, 106(2012):261–274.
[Crossref] [Google Scholar] [PubMed]
- B. Joob, V. Wiwanitkit, Emerging of cysticercosis in Europe: A concern, Acta Neurol Belg, 112(2012):427.
- S. Fabiani, F. Bruschi, Neurocysticercosis in Europe: Still a public health concern not only for imported cases, Acta Trop, 128(2013):18–26.
[Crossref] [Google Scholar] [PubMed]
- K. Kanobana, A. Ruiz, L. Rojas, R. Andrade, F. Rosado, et al. Taenia solium cysticercosis: The case of Cuba, PLoS Negl Trop Dis, 7(2013):e2202.
[Crossref] [Google Scholar] [PubMed]
- V. Wiwanitkit, Neurocysticercosis: Control and eradication, Salud Publica Mex, 55(2013): 246.
- L. Zammarchi, A. Angheben, F. Gobbi, G. Zavarise, A. Requena-Mendez, et al. Profile of adult and pediatric neurocysticercosis cases observed in five Southern European centers, Neurol Sci, 37(2016):1349–1355.
[Crossref] [Google Scholar] [PubMed]
- S. Gabriël, P. Dorny, K. E. Mwape, C. Trevisan, U. C. Braae, et al. Control of Taenia solium taeniasis/cysticercosis: The best way forward for sub-Saharan Africa?, Acta Trop, 165(2017):252–260.
[Crossref] [Google Scholar] [PubMed]
- M. Laranjo-González, B. Devleesschauwer, C. Trevisan, A. Allepuz, S. Sotiraki, et al. Epidemiology of taeniosis/cysticercosis in Europe, a systematic review: Western Europe, Parasit Vectors, 10(2017):349.
[Crossref] [Google Scholar] [PubMed]
- C. Trevisan, S. Sotiraki, M. Laranjo-González, V. Dermauw, Z. Wang, et al. Epidemiology of taeniosis/cysticercosis in Europe, a systematic review: Eastern Europe, Parasit Vectors, 11(2018):569.
[Crossref] [Google Scholar] [PubMed]
- J. Iqbal, S. Ahmad, M. Al-Awadhi, A. Masud, Z. Mohsin, et al. A large case series of neurocysticercosis in Kuwait, a nonendemic Arabian gulf country in the Middle East region, Microorganisms, 9(2021):1221.
[Crossref] [Google Scholar] [PubMed]
- R. D. Hernández-Chea, P. Morales-Ramírez, M. Hernández, A. Toledo, A. Hun, et al. Taenia solium taeniasis/cysticercosis in Guatemala: A prevalent public health problem?, Pathog Glob Health, 117(2023):5–13.
[Crossref] [Google Scholar] [PubMed]
- H. Carabin, A. A. Traoré, Taenia solium taeniasis and cysticercosis control and elimination through community-based interventions, Curr Trop Med Rep, 1(2014):181-193.
[Crossref] [Google Scholar] [PubMed]
- S. Gabriël, M. V. Johansen, E. Pozio, G. S. A. Smit, B. Devleesschauwer, et al. Human migration and pig/pork import in the European Union: What are the implications for Taenia solium infections?, Vet Parasitol, 213(2015):38-45.
[Crossref] [Google Scholar] [PubMed]
- Carpio, A. Fleury, M. L. Romo, R. Abraham, Neurocysticercosis: The good, the bad, and the missing, Expert Rev Neurother, 18(2018):289-301.
[Crossref] [Google Scholar] [PubMed]
- H. A. Ngowi, A. S. Winkler, U. C. Braae, R. H. Mdegela, E. M. Mkupasi, et al. Taenia solium taeniosis and cysticercosis literature in Tanzania provides research evidence justification for control: A systematic scoping review, PLoS One, 14(2019):e0217420.
[Crossref] [Google Scholar] [PubMed]
- CystiTeam Group for Epidemiology and Modelling of Taenia solium Taeniasis/Cysticercosis. The World Health Organization 2030 goals for Taenia solium: Insights and perspectives from transmission dynamics modelling, Gates Open Res, 3(2019).
[Crossref] [Google Scholar] [PubMed]
- M.-B. Qian, N. Xiao, S.-Z. Li, B. Abela-Ridder, H. Carabin, et al. Control of taeniasis and cysticercosis in China, Adv Parasitol, 110(2020):289-317.
[Crossref] [Google Scholar] [PubMed]
- R. Kaur, N. Arora, S. S. Rawat, A. K. Keshri, S. R. Sharma, et al. Vaccine for a neglected tropical disease Taenia solium cysticercosis: Fight for eradication against all odds, Expert Rev Vaccines, 20(2021):1447-1458.
[Crossref] [Google Scholar] [PubMed]
- M. A. Dixon, P. Winskill, W. E. Harrison, M.-G. Basáñez, Taenia solium taeniasis/cysticercosis: From parasite biology and immunology to diagnosis and control, Adv Parasitol, 112(2021):133-217.
[Crossref] [Google Scholar] [PubMed]
- N. Nekrasova, O. Tovazhnyanska, D. Sushetska, O. Markovska, A. Shapkin, et al. Neurocysticercosis with symptomatic epilepsy manifestation, Med Glas (Zenica), 18(2021):444-449.
- Z. Nsadha, C. Rutebarika, C. Ayebazibwe, B. Aloys, M. Mwanja, et al. Control trial of porcine cysticercosis in Uganda using a combination of the TSOL18 vaccination and oxfendazole, Infect Dis Poverty, 10(2021):34.
[Crossref] [Google Scholar] [PubMed]
- G. Cárdenas, P. Salgado, E. Laura-Foronda, I. Popoca-Rodriguez, R. D. Delgado-Hernández, et al. Neglected and (re-emergent) infections of the CNS in low-/middle-income countries, Infez Med, 29(2021):513-525.
[Crossref] [Google Scholar] [PubMed]
- H. H. Garcia, A. E. Gonzalez, R. H. Gilman, Neurocysticercosis as an eradicable cause of epilepsy: A plan and actions are needed, JAMA Neurol, 78(2021):1045-1046.
[Crossref] [Google Scholar] [PubMed]
- L. E. Jerez Puebla, F. A. Núñez Fernández, J. Fraga Nodarse, R. Cordovi Prado, I. A. Millán, et al. A retrospective study of Taenia spp. in Cuban patients: What does molecular analysis tell us?, Food Waterborne Parasitol, 25(2021):e00136.
[Crossref] [Google Scholar] [PubMed]
- R. Pineda-Reyes, A. Clinton Jr White, Neurocysticercosis: An update on diagnosis, treatment, and prevention, Curr Opin Infect Dis, 35(2022):246-254.
[Crossref] [Google Scholar] [PubMed]
- M. S. Hossain, S. Shabir, P. Toye, L. F. Thomas, F. H. Falcone, Insights into the diagnosis, vaccines, and control of Taenia solium, a zoonotic, neglected parasite, Parasit Vectors, 16(2023):380.
[Crossref] [Google Scholar] [PubMed]
- Valdés Lourdes Fátima, H. Foyaca Sibat, The Role of Oxidative Stress in Neurocysticercosis: A Comprehensive Research, Clin Schizophr Relat Psychoses, 17(2023).
- Valdés Lourdes de Fátima, D. Thozama, H. Foyaca Sibat, Neuropsychiatric manifestation in neurocysticercosis, J Drug Alcohol Res, 12(2023):11.
- Valdés Lourdes de Fátima, H. Foyaca Sibat, Ferropanoptosis in neurocysticercosis: A comprehensive research, Clin Schizophr Relat Psychoses, 17(2023).
- M. Nico Garcia, I. Valdés Lourdes de Fátima, H. Foyaca-Sibat, Our Hypotheses about the Role of Cuproferropanoptosis in Neurocysticercosis and a Comprehensive Review, J Drug Alcohol Res, 12(2023):9.
- Valdés Lourdes de Fátima, H. Foyaca Sibat, Novel hypotheses on the role of oligodendrocytes in neurocysticercosis: A comprehensive research, Clin Schizophr Relat Psychoses, 17(2023):17.
[Crossref]
- Valdés Lourdes de Fátima, H. Foyaca Sibat, New hypotheses on the role of microglias in Ischemic Reperfusion injury secondary to neurocysticercosis, Clin Schizophr Relat Psychoses, 17(2023).
- L. de Fátima Ibañez Valdés, The role of rouget cells in neurocysticercosis, J Drug Alcohol Res, 13(2024):17.
- L. de Fátima Ibañez Valdés, H. Foyaca Sibat, Obstructive sleep apnea syndrome and neurocysticercosis, J Drug Alcohol Res, 13(2024):14.
[Crossref]
- Fátima Ibañez Valdés, H. Foyaca Sibat, Comorbidity of alcohol use disorder and neurocysticercosis aggravated by dysbiosis, J Drug Alcohol Res, 13(2024):8.
[Crossref]
- de Fátima Ibañez Valdés, H. Foyaca, Pathophysiology of Cerebral Cysticercosis Related to PANoptosis, Microglia Polarization and Novel Drugs Implications, J Drug Alcohol Res, 14(2025):13.
[Crossref]
- H. Foyaca Sibat, L. de Fátima Ibañez Valdés, Introduction to Cysticercosis and Its Historical Background, Novel Aspects on Cysticercosis and Neurocysticercosis, Prof. Humberto Foyaca Sibat (Ed.), InTech, (2013).
[Crossref]
Copyright: © 2025 Lourdes de Fatima Ibanez Valdes, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.