Research Article: Journal of Drug and Alcohol Research (2023) Volume 12, Issue 9
A Systematic Review on Controlled Porosity Osmotic Drug Delivery System: Recent Developments and Future Prospects
Voleti Vijaya Kumar and Ismail Y*Research Scholar, Crescent School of Pharmacy, B.S. Abdur Rahman Crescent Institute of Science and Technology, GST Road, Vandalur, Chennai, Tamil Nadu, India
Ismail Y, Research Scholar, Crescent School of Pharmacy, B.S. Abdur Rahman Crescent Institute of Science and Technology, GST Road, Vandalur, Chennai, Tamil Nadu, India, Email: Ismailcsp@crescent.education
Received: 02-Oct-2023, Manuscript No. JDAR-23-116175 ; Editor assigned: 04-Oct-2023, Pre QC No. JDAR-23-116175 (PQ); Reviewed: 18-Oct-2023, QC No. JDAR-23-116175; Revised: 23-Oct-2023, Manuscript No. JDAR-23-116175 (R); Published: 30-Oct-2023, DOI: 10.4303/JDAR/236261
Abstract
Objective: The current review's aim was to further explain the recent technologies adopted to develop Osmotic Drug Delivery System (ODDS).
Significance: A high quantity of In-Vitro and In-Vivo Correlation (IVIVC) is expected in ODDS.
Methods: The current review provides an overview of the fundamentals of ODDS, types, with a focus on Controlled Porosity Osmotic Pumps (CPOPs), components, suitable drug candidates, formulation strategies, coating materials, and commercially available preparations based on these systems. We have reviewed Artificial Intelligence (AI) and robotic technology, how it can be employed for designing ODDS.
Results: Osmotic systems' predicted release rate may be planned by altering the release control settings. The achievements of this medication delivery in the present and the future is indicated by the products now on the market, the patents filed thus far, and the efficacy discovered for osmotic products.
Conclusion: A promising approach for oral medicine administration is ODDS, these formulations comprising the osmotic agent, pore forming, and rate-controlling membrane can be designed using controlled porosity osmotic technology. The regulation of medication release according to the required time period can be achieved by optimizing these parameters. This method enables the release to be pulsed during a defined period of chronotherapy.
Keywords
Osmotic Drug Delivery Systems (ODDS); Osmotic pump; Chronotherapy; Colon Targeting and Osmotic pressure
Introduction
Novel Drug Delivery System (NDDS) is a different way of administering medication than conventional drug delivery systems [1]. Oral drug delivery looks to be a successful method for giving a range of drugs due to its efficiency and ease in delivering to sick people [2]. Because it is inexpensive and simple to provide to patients, the oral route is a practical way to administer a variety of medications. However, the quick release of drugs is provided by traditional delivery systems, which do not regulate drug’s release. Chemical/Physical attributes of the substance, the occurrence of emigrants, physical factors including the inclusion or exclusion of nutrition, the ionic strength of the gastroenteritis mucosa, the gastro intestinal flagella, and other factors influence the speed as well as the scope of systemic absorption through repeated tasks. Researchers have concentrated on developing NDDS to address these issues [3]. The regulated drug delivery secretion system offers benefits in patient compliance, ease, but also reduces via variations inside a steady flow blood stage, among other models like innovative DDS which are currently in the market. Controlled Drug Delivery System (CDDS) reduces the overall dose while maximizing drug use and distributes medicines with shorter half-lives. The release of a drug can be controlled both temporally and spatially with CDDS. But among the most cutting-edge DDS, the ODDS, uses osmotic pressure as a prime factor for the regulated distribution of pharmaceuticals [4]. Release of medications from the system is not affected by the inclusion or exclusion of nutrition, the acidity of the GIT, GI movement, or the hydrodynamic environment of the body owing to a rate-regulating selectively-permeable barrier. To keep drug concentrations within the therapeutic window, the dosage and frequency are adjusted in ODDS [5]. Over an extended length of time, ODDS provides the medication at a predefined zero order rate. In order to ensure consistent drug delivery, it serves as the standard formulation. ODDS would offer a standardized substance concentration at the location of permeation, and since permeation permits maintaining plasma levels within the recommended dose, which also reduces adverse effects but also prevents the intensity of administering medication, they would be useful for delivering medications. Water diffuses into the center of an osmotic system upon contact with water, creating an osmotic gradient that regulates the release of the medicine [6]. The amount of medication administered via osmotic devices is controlled by osmotic pressure, which is created when fluids from of the surrounding environment is absorbed into the dosage form [7,8]. The force onto the side of a semipermeable membrane with a higher solution concentration to avoid water from going through is known as osmotic pressure. The osmotic pressure produced by the osmogen’s fluid absorption is inversely linked to the pace of drug delivery from its formulation. The ODDS has a strong in vitro-in vivo connection. Therefore, of all the methods, osmotic drug distribution is the most intriguing and well-liked [9]. Some of the commercially available ODDS are shown in Tables 1-3.
Table 1: commercially available ODDS products
| Brand | Active ingredient | Design | Dose |
|---|---|---|---|
| Acutrim | Phenylpropanolamine | Elementary pump | 75 mg |
| Alpress LP | Prazosin | Pushâ??pull | 2.5 mg-5 mg |
| Cardura XL | Doxazosin | Pushâ??pull | 4 mg, 8 mg |
| Covera HS | Verapamil | Push-pull with time delay | 180 mg, 240 mg |
| Glucotrol XL | Glipizide | Push-pull | 5 mg, 10 mg |
| Efidac 24 | Chlorpheniramine maleate | Elementary pump | 4 mg IR, 12 mg CR |
| Efidac 24 | Pseudoephiderine | Elementary pump | 60 mg IR, 180 mg CR |
| Dynacirc CR | Isradipine | Push-pull | 5 mg, 10 mg |
| Ditropan XL | Oxybutinin chloride | Push-pull | 5 mg, 10 mg |
Osmotic drug delivery system
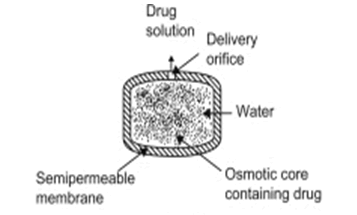
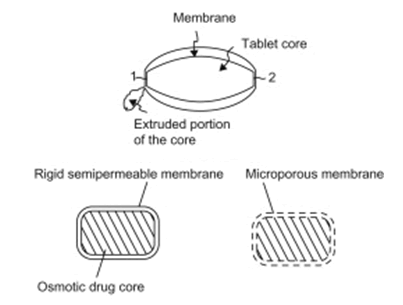
The fundamental idea behind an osmotic medication delivery system is that solvent particles circulate throughout the system until an equilibrium concentration is reached on both sides. In chronic conditions, where osmotic pressure serves as a propellant for medication release into systemic circulation, this process regulates drug release and aids in reducing the need for repeated drug administration. This procedure operates in accordance with zero order kinetics and skips the first pass metabolism without accessing the liver, allowing for a reduction in the amount of dosage administered (Figure 1).
Table 2: Various types of OOPs
| Osmotic system | Similarities | Differences |
|---|---|---|
EOP
|
Osmotic core Water flow is regulated by a semipermeable membrane. |
Single layer tablet A single tiny orifice Drug dispersed in the form of solution |
Push-pull
|
Bilayer tablet mostly latitudinallycompressed Both layers contain an osmotic agent. Few tiny orifices Drug dispersed in a suspension or solution form |
|
Push-stick
|
Bilayer tablet longitudinally compressed Push layer contains osmotic agent A single big orifice Drug is discharged as a moist material that must be afterwards broken down and dissolved. |
|
EnSoTrol
|
Single layer tablet Few tiny orifices Integration of a wicking agent and a solubility enhancer Drug dispersed in the form of solution |
|
Controlled Porosity and Single Composition Osmotic Tablet (SCOT)
|
Single layer tablet There isn't a predrilled orifice. Drug delivered via in-place channels or crevices as a solution or moist material. |
|
L-OROS
|
Single softgel capsule A single tiny orifice Drug disperses in the form of liquid |
Table 3: Criteria and specifications of CPOPs
| Excipient | Specifications |
|---|---|
| Plasticizer and flux regulating agent | 0-50, mostly 0.001-50 parts per 100 parts of wall material |
| Surfactants | 0-40, most commonly 0.001 to 50 parts per 100 parts of wall material |
| Wall thickness | 1 mm-1000 mm, most commonly 20 mm-500 mm |
| Osmotic pressure | 8 atm-500 atm |
| Core size | 0.05 mg-5 g |
| Micro porous structure | 5%-95% pores should have 10 mm-100 mm diameter, 0.1%-60% mostly have 0.1%-50% by weight depending onoverall weight of additives and polymer. |
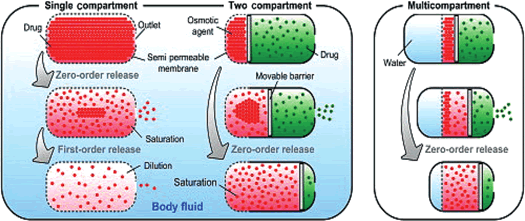
Figure 1: ODDS
ODDS devices
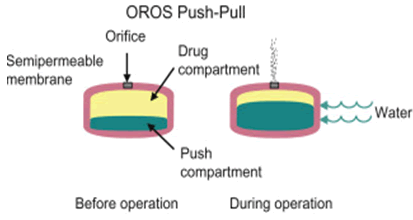
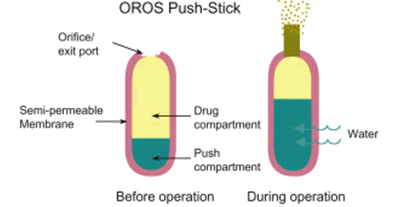
The following categories of ODDS may be determined by the design of the devices and their current state of use [10] (Figure 2).
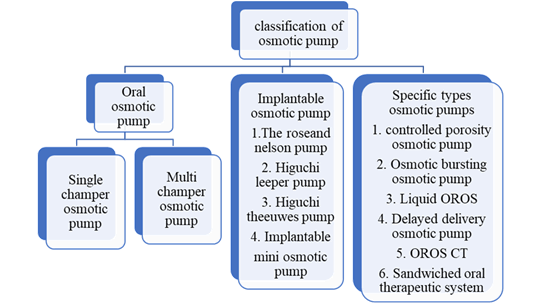
Figure 2: Types of osmotic pump
Implantable osmotic pump
An osmotic engine, a cavity that partly encloses the engine, and a piston that is contained inside the compartment are all components of an implantable osmotic pump that delivers medication. Osmotic engine can be utilized to push the piston inside the chamber and eject the active component when the pumps are implanted in an aquatic environment. The Higuchi euwes pump, and the Alzet and Duros small osmotic pump are a few examples of different implantable osmotic systems [11] (Figures 3 and 4).
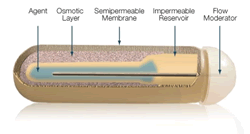
Figure 3: Implantable osmotic pump
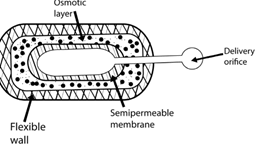
Figure 4: Higuchi theesue osmotic pump
Mechanism: Salt utilized in the salt compartment and the membrane’s permeable properties control how quickly the drug leaves the ODDS. The delivery port is designed to resemble a long, thin tube to reduce the drug’s diffusional leakage.
Application: They commonly serve as implanted controlled release delivery systems in research projects that require continual medication administration (Figure 5).
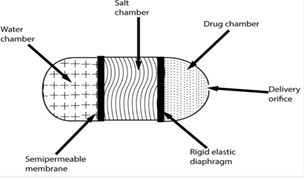
Figure 5: Rose nelson pump
Mechanism: The compartment containing the salt and water is divided by a selectively-permeable membrane. Pressure differences have an impact on how water moves from its chamber into the adjacent chamber. Drug is finally pushed out of the system. It is feasible that the water movement that lowers the latex diaphragm into the compartments causes the salt chamber’s volume to grow (Figure 6).
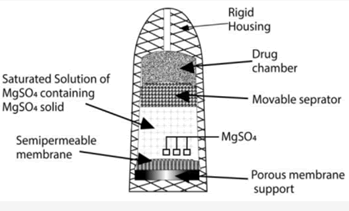
Figure 6: Higuchi Leeper pump
Mechanism: It lacks a water compartment; instead, it activates when water from the surroundings is absorbed. This modification enables the preparation of the device filled with medication and permits for long-term storage before use.
Application: Higuchi-leeper pumps are often used in veterinary settings.
Oral Osmotic Pump (OOP)
A patient’s mouth is filled with an active chemical using an OOP, which is an osmotic device. With a shaped semipermeable barrier, the osmotic device encloses a section encompassing water-insoluble drug material. A channel running across the semipermeable membrane links the compartment housing the drug, for transferring the chemical from the equipment to the outside of the device. According to the number of chambers in the OOPs, multi chamber pumps include the Push-Pull Osmotic Pump (PPOP), the Elementary Osmotic Pump (EOP), and the osmotic pump having a non-expanding chamber [12] (Figure 7). Oral osmotic pump-e.g., Procardia XL for nifidipine.
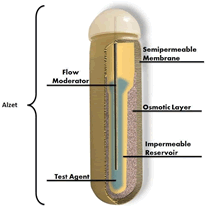
Figure 7: Oral osmotic pump
Advantages: Provide both extremely water soluble (oxybutynin hydrochloride), and almost insoluble substances.
Mechanism: Osmotic pressure gradient causes water to be absorbed via the SPM, generating a saturated drug solution within the system. Due to the increased hydrostatic pressure within the tablet, the saturated solution is forced to pass through the orifice in the film.
Specific types
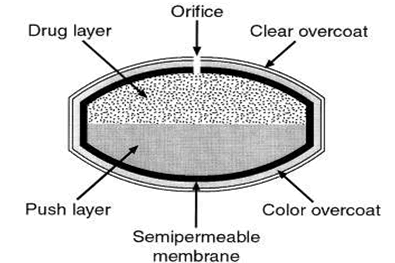
Recently developed osmotic pump systems includes the CPOP, the liquid OROS/liquid oral osmotic system, the Osmotic Bursting Osmotic Pump (OBOP) for example lipid osmotic pump, pulsatile delivery having expandable orifice, Telescopic capsule, OROS CT, monolithic osmotic system, osmatic multi-particulate delayed release systems, sandwiched osmotic tablets, pulsatile delivery by aseries of stops, and are some examples of the CPOP hard, soft, and delayed liquid bolus delivery systems [13-15].The most reliable drug delivery method in CDDS is the oral treatment dose strategy. These dosage forms use osmotic pressure as its primary mechanism for releasing the medication in a regulated manner (Figure 8). The reasoning behind these systems’ ability to distribute the medicine in a regulated way is. In “Osmotic Pump Tablets (OPT),” the core drug layer, also known as the active pharmaceutical component or the drug(s), is often covered by a second layer acting as an osmotic agent, various additives, and a coat of a transparent semipermeable layer. According to zero-order kinetics, this process entails the achievement of the process of development in innovative pharmacological dosage forms. This gives the system a push to release the active medicinal ingredient. Osmotic pump tablets work by using the osmotic pressure principle on the grounds of a differential across the membrane and inside the membrane.
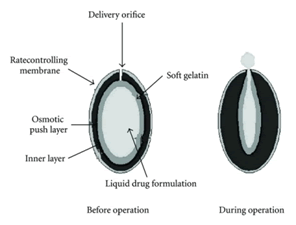
Figure 8: OROS oralosmoticsystem
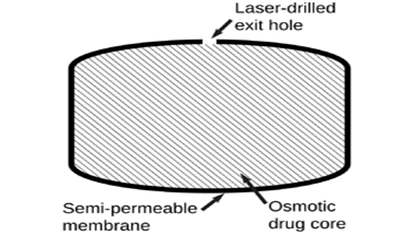
Controlled Porosity Osmotic Drug Delivery (CPODD)
Controlled Porosity Osmotic Pump (CPOP): Principle: The medicine is delivered in an asymmetrical manner using this system’s single and multiple-compartment administration options. It has a thin covering that is kept in place by a porous structure. By combining a mixed solvent solution and a phase inversion mechanism, this membrane is created. This membrane prevents the solute particles from passing through, but it allows the solvent particles, such water, to pass through the layer and release the medication. This process results in the creation of the sponge structure, which results in controlled porosity. Incorporated by RW Hartnett Numerous factors, including the semi-permeable membranes water permeability process, the coating layer’s thickness, the solubility of the coating layers components, this release process is observed using the drug’s solubility in central compartment and the consistency of the osmotic pressure sustained between the layers [16]. This technique is independent of variables such as pH, medium movement, and osmotic pressure of the formulations, the total surface area, and layer coat thickness. The process of drug release from the CPOP may be triggered by these unbalanced conditions [17].
Controlled Porosity Osmotic Pump Tablet (CPOPT):
It is the most basic type of osmotic pump. CPOP tablets, which contain the drug in an insoluble coating polymer and water soluble polymers, were created to aid in managing the porosity osmotic drug delivery method in this model. This has an uneven structure and is maintained by a thin covering membrane with a porous character [18]. The coating layer is permeable to water and can develop pores, but it is not affected by the solute absorption additive that is spread across the membrane layer. The membrane, which were water permeable, spills out dissolved polar-soluble additives when it is exposed to an aqueous environment. These outcomes lead to the production of a sponge-like structure (microporous membrane), which is porous and permeable but resistant to the absorption of solutes. Typically, components obtained from pores with a size range of 5% to 95% between and 100 m are examined to find drugs with a moderate to high solubility release mechanism employing a variety of solubility modulators. Mannitol, sorbitol, urea, KCl, NaCl, etc., are employed as potential pore-forming excipients. The frequency of medicine deliveries from this system depends on the number of coatings, the quantity of soluble components it contains, the semipermeable membrane’s permeability, the absorption of medication through the tablet core, the osmotic force difference on either side of membrane, and the coating’s total surface area, but it is unaffected by pH or agitation of the release media. The above performance is durable since the designer has control over these variables and they don’t change under physiological circumstances.
Mechanism of CPOPT: The drug is released through a semipermeable membrane in a regulated manner in a CPOPT owing to the osmotic pressure gradient between exterior fluid and drug-compartment found in the tablet’s drug delivery system [19]. The distribution technique at both forms includes a core containing the medication that is bound by a coating layer. The pump is made up of dosage forms with one or more compartments [20]. Layer is not penetrable for the solute and water-permeable with the addition of an additive that distributes insensitive holes throughout the layer. The CPOP tablet’s drug release mechanism involves a semi-permeable membrane that allows water-permeable polymer compounds to enter the tablet core. Drug and other soluble elements dissolve in the core, then, it is pushed out of holes when water comes into contact with tablet. The difference between the thermodynamic activity of the membrane and the flow of an osmotic agent between the core and an external medium, such as the fluids of the stomach or intestines or the receptor solution. The resulting sponge-like structure, which was also remarkably permeable to both dissolved pharmaceutical compounds and water, eventually forms the controlled porosity walls of interest. The core’s soluble components disintegrate, resulting in an activity gradient and an osmotically distinct core from its surroundings (Figure 9).
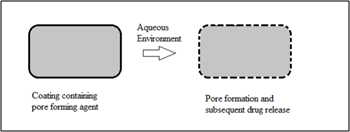
Figure 9: Controlled porosity osmotically delivery system
The amount of drug solution administered would be nearly equivalent to the quantity of water absorbed in the allotted amount of time, as per the concept of constant dosage form volume. Across the membrane, the amount of additional water causes a change in hydrostatic pressure, as it works its way into the centre and forces the solutions out through the coating’s pores. Since the membrane’s penetration property is stable, the drug quantity in the excluded solution is fixed, and the pressure difference on either side of membrane is maintained continuously, drug delivery rate will also remain fixed. Persistent drug release following zero-order kinetics may be attained using membrane devices which are asymmetric, at the same time the for the soluble drug concentration the fluid component of the core doesn’t change. Release rate declines, as the drug quantity in the core depletes of saturation point. The drug delivery rate is based on various types of properties such as aqueous permeation though semi porous layer, osmotic pressure of the formulation and overall coating surface area and thickness. These variables must be under the developer’s control and do not change with physiological circumstances. The formula may be employed to represent the device’s water flow rate
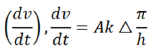
dv/dt=movement of solvent around the membrane A
h=coating layer thickness
k=permeability of membrane in cm2,
A=membrane area
Δπ=Difference in osmotic layer.
The above equivalence insistently aimed at entirely semipermeable layer in which membrane remains completely impermeable towards osmotic agent but then permeable towards water [21].
There are a number of apparent advantages intrinsic to the controlled porosity osmotic pump system. Considerable issues with stomach squeezing are decreased by means of dosage release process though entirely rather than from the device surface compared to one hole. Furthermore, since the holes are produced in place, a sophisticated laser drilling unit is not necessary.
Advantages: Drug release rate is monitored by zero order kinetics especially in CPODD. The main advantages are:
• By comparing to conventional dosage forms this dosage forms provides enhances bioavailability of the drug.
• Pulsatile DDS could help in delay in the drug releasing process.
• As this system follows zero order kinetics it is not dependent on variables like GI PH, body’s physiological conditions like temperature, climatic condition etc.
• In-vitro and In-vivo correlation was found to be very significant in this drug delivery system.
• By comparing to other dosage forms in this dosage form food is showing less action in the drug release and action process.
• In situ drilling process is carried out in this CPODD delivery system hence no need of drilling process using special equipment.
• Less GI irritation is identified.
• Drug delivery is carried out through surface layer of the dosage form there by there will not be any issue of drug release process through orifice
• This dosage preparation is very easy than compare other novel drug delivery systems
• This formulation design is compatible to all types of soluble drugs [22,23].
Disadvantages:
• This method requires some trained person and process should be designed in a effective manner.
• With drawing of therapeutic effect is not possible, once the releasing process is processed.
• If coating process is not in the proper manner then chance of dose dumping takes place and it may lead improper drug release rate [23].
• Drug tolerance development process is more than compare to other dosage forms (Figure 10).
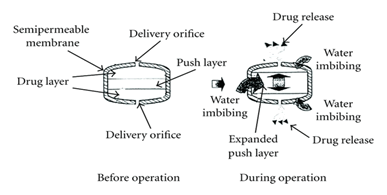
Figure 10: Elements of osmotic system
In osmotic systems drug is an important content used as long life treatment and have short half-life. A diversity of drugs like Nifedipine, Calcium channel blockers like diltiazem hydrochloride, Angiotensin conversion enzymes like oxprenolol, metaprolol, glipizide and Carbamazepine can be prepared using this advance ODD system [24,25].
Osmotic components/osmogens: They sustain a concentration difference throughout the membrane in order to produce osmotic compositions. They dissolve in biological fluid during penetration of the CPOP across semi permeable membrane, creating an osmotic pressure in the pump and pushing medication out through delivery aperture [26]. They function as a catalyst for water absorption and aid in upholding the homogeneity of the drug in the aqueous formulation. They are employed in the designing of customized mechanisms for extended release of relatively drugs with weak aqueous solubility and ODDS. Polymer-derived osmogens are largely utilized in the formulation of CPOP. In the concentration solution, osmogents produce osmotic pressures between 8 atm and 500 atm [27]. The osmogents classification is tabulated in Table 4.
Table 4: Types of osmogents
| Category | Examples |
|---|---|
| Water soluble salts of organic acids | Pot. acetate, Sod. ascorbate |
| Sod. acetate, Sod. citrate | |
| Sod. benzoate | |
| Water soluble salts of inorganic acids | NaCl, Mag. chloride |
| Pot. sulphate | |
| Mag. sulphate, KCl | |
| Sod. bicarbonate | |
| Weak acids | Tartaric acid, Melanic acid, Citric acid |
| Fumaric acid | |
| Organic polymeric osmogents | HPM |
| CMC | |
| HEMC | |
| Cross linked PVP | |
| Water soluble amino acids | Leucine, Glycine, Methionine, Alanine |
| Carbohydrates | Mannitol, Arabinose, Dextrose, Sucrose |
| Glucose, Lactose, Galactose, Fructose, Maltose, Xylose, Sorbitol |
Semipermeable layer: A crucial component of this osmotic delivery mechanism is semipermeable. This makes the decision to use a polymer-based membrane in the osmotic delivery formula critical. The membrane’s impermeabilities to the flow of medications and other elements found in the chambers is one of its characteristics. Due to its inertness and ability to keep its dimensional integrity throughout drug delivery, semipermeable materials provide a steady pushing force. Which kind of polymer A covering material used in osmotic processes may be impermeable to solute and permeable to water. Examples of cellulose esters particularly, ethyl cellulose, eudragits, and cellulose tri acetate [28].
Agents that regulates flux: The layer of the osmotic Delivery methods can be created by using flux regulating agents to regulate the fluid permeability. Some of the hydrophilic substances like polyhydric alcohols, polyalkylene glycols, polyethylene glycols (300 Da-6000 Da) improves the flux, the hydrophobic substances, such as dimethoxyethylphthalate or diethyl phthalate, and have the tendency to reduce flow when substituted with an alkyl or alkoxy group. The water-impermeable compounds such as insoluble salts or insoluble oxides can also be employed for this purpose [29].
Water penetrating agents (wicking agent): It is considered as a substance that helps to illustrate liquid into a delivery device’s porous structure. A wicking agent can either swell or not depending on its composition. The characteristic of wicking agent is physisorption with liquid, which is a type of absorption in this the surfaces of the wicking agents holds the solvent molecules loosely by vander waals interactions between surfaces of the absorbed molecules and wicking agents. The purpose of this excipient is to move the water towards the tablet core’s surfaces, establishing channels that increase the surface area. Poly Vinyl Pyrrolidine (PVP), Sodium dodecyl sulfate, alumina, Kaolin, titanium dioxide, colloidal silicon dioxide, m-pyrrole, magnesium aluminum silicate, bentonite, polyester, and polyethylene are among the resources that are effectively active as wicking agents [30].
Agents helping for pores formation process: In case of low aqueous soluble active molecules pumps develops pore forming agents in a predominant manner. Also used in even release “controlled porosity” and by the process of “Multi particulate osmotic pumps”. By the development of the microporous membrane uses pore-forming substances the micro porous wall may be generated on-site while the device is operating thanks to pore former bolting [31]. The pore forming may be solid, liquid, inorganic, or both. Carbohydrates including sucrose, lactose, glucose, mannose, fructose, mannitol, sorbitol, and diols as well as polyols like poly vinyl pyrrolidine and poly-hydric alcohols are all examples of alkaline earth metals are a few examples of pore-forming substances [32]. The pore forming agent’s classification is shown in Table 5.
Table 5: Classification of pore forming agents
| Type | Examples |
|---|---|
| Proteins | Bovine Serum Albumin (BSA) |
| Carbohydrates | Fructose, Sorbitol, Mannitol, Sucrose, Glucose, Lactose, Mannose, Pentaerythritol |
| Alkaline metals | CaCl2, Calc. Nitrate |
| Alkaline salts | Sod. Bromide, NaCl, Pot. Sulphate, KCl, Pot. Phosphate |
| Phthalate derivatives | Dibutyl Phthalate (DBP), Diethylphthalate |
| Diols and polyols | PEG, PVP, PVA |
Coating solvent: The coating solvents which are useful for developing polymeric solution that solution is employed for making the osmotic device barrier [33]. Solvents include organic or unlike organic solvents, inorganic solvents will not seriously destruct the core, wall, or other parts. The traditional solvents include water, ethanol, isopropyl alcohol, methylene chloride, ethyl acetate, acetone, butyl alcohol, carbon tetra chloride, and methanol. It can use mixtures of solvents like methylene chloride and methanol (79:21), acetone and ethanol (80:20), acetone and methanol (80:20), acetone and water (90:10), and so on [34].
Emulsifying agents: In order to create an integrated composition for creating the device’s wall, emulsifying agents are combined with the wall-forming substance. These agents uphold the surface energy of the components to enhance the ingredients’ integrating into the formulation and uphold their stability during the surroundings of usage throughout the drug release phase [35]. A few examples of emulsifying agents include polyoxyethylenatedglycerylrecinoleate, polyoxyethylene castor oil containing glycerol (sorbitanoleate, stearate, or laurate), ethylene oxide, and glyceryl laureates.
Plasticizers: Plasticizers are significant important in the osmotic systems formulation development and various kinds then quantities in the ratio of plasticizers used for the coating layer process. The plasticizers contain change in the visco-elastic action properties of “polymers” this variations result might influence polymeric film permeation process. Some plasticizers are used for low permeability such as Polyethylene glycols, “Ethylene glycol monoacetate”; then other form as Diacetate of ethylene glycol, try ethyl citrate, Diacetin or diethyl tartarate helps for more improving the permeation process [36].
Barrier layer formers: Barrier formers provide the twin functions of isolating the drug layer from the osmotic barrier and prevent water from entering certain parts of the delivery mechanism. High density polyethylene, wax, rubber, and other materials are examples of barrier layer formers [37].
Evaluation of ODDS
Compatibility studies: Fourier Transforms Infrared Spectroscopy (FT-IR): FTIR technique can be used to highlight the impact of various functional groups of drugs and additives, by examining the major variations in the form and location of absorbance bands. This process involved grinding and completely combining the drug and excipient mixture with KBr (1:100) for 3 min to 5 min using a mortar, followed by compressing the mixture into a disc in a hydraulic press for 5 min, less than 5 tons of pressure. Sample with KBr pellet was held in the sample holder while being scanning in FT-IR spectrophotometer from 4000 cm-1 to 400 cm-1. The peaks of the improved formulation were then contrasted with those of the pure drug and additives. When no interactions existed between both the drug’s peak concentration and the inactive ingredients in the optimized formulation, it was regarded as compatible [38].
Differential Scanning Calorimetric Analysis (DSC): Using DSC, the drug’s compatibility with other ingredients (additives) was evaluated. Physical mixes of the drug and several additives were taken and assessed with DSC in a 1:1 ratio. In a DSC pan, individual samples and physical mixes of the medication and additives were weighed to a maximum of 5 mg. For efficient heat conduction, the sample pan was crimped. It was then scanned from 50 C to 3000 C. The thermogram that resulted from the application of a 20 cm-1 heating rate was investigated for any signs of interactions. Finally, a comparison between the thermograms of pure samples and an optimised formulation was made [39].
Evaluation of osmotic pump tablets: Pre-compression parameters: Angle of repose (θ): The method utilized to generate the heap has a significant impact on the angle of repose test. Measuring the heap shape can help calculate the angle of repose (θ). θ may be computed by applying the conventional technique [40]. Initialization tube rises at a steady rate of 5 mm/s after being manually filled with a sample of powder. As a result, a pile of powder emerges from the tube and rests on the cylinder-shaped support. Slowly, this support rotates about its axis. Various orientations of the heap are captured using a CCD camera. Images were recorded and rotated by 22.5⁰ to achieve the results shown in the following section. The entire geometrical data was retrieved in this manner. By using image analysis, the heap algorithm determines the location of the powder/air contact from each photo. The isosceles triangle, having surface area is equivalent to that of the heap, has an angle of repose (θ). The following equation is used to determine θ and measure the diameter of powder heap.

Where θ represents the angle of repose, h and d indicate the height of heap and diameter of the circular support (cm).
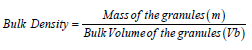
Bulk density: Granules are poured into a measuring cylinder to calculate bulk density. Granules’ mass (m) and bulk volume (Vb) are calculated. The following formula is used to determine the bulk density [41].
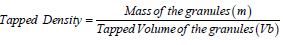
Tapped density: Graduated cylinder is tapped 1,000 times for a predetermined amount of time while encompassing a definite quantity of granule blend. Both the granular mass (m) and the minimal volume of the cylinder that is occupied (Vt) are weighed [42].The formula below may be utilized for computing the tapped density.
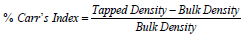
Compressibility index (Carr’s index): Flow properties of the granules created by Carr are determined by the Carr’s index. Granules’ % compressibility is a potential indicator of the stability and potential arch of the powder [43]. Calculating the Carr’s index is possible. The equation below may be used to determine the Carr’s index.
Hausner’s ratio: For determining the flow characteristics of granules, one uses Hausner’s ratio. Calculate it by adding the tapped density to the bulk density ratio [44].
Post compression parameters
Thickness: Vernier calipers are used to measure the thickness of individual tablets because they provide a precise measurement of thickness. It details how different osmotic pump tablets differ in thickness. Typically, mm is used to measure thickness. Each tablet’s maximum thickness variance is 5%.
Hardness: By utilizing the Monsanto hardness tester and measuring in kg/cm2, the hardness of tablets can be determined [45].
Friability: Tablet friability was carried out in a Roche friabilator. Ten pills were inserted in the chamber after being jointly weighted (disseminated in an insoluble). The test involves dropping the tablets from an altitude of six inches with each cycle of the friabilator, which was run for 100 revolutions, subjecting them to the cumulative effects of friction and shock. Then, tablets are powdered and weighed once again (W) [46].
Weight variation: In weight variation test, 10 tablets were weighed separately, their mean is determined, and the separate tablet weights are comparing to the mean. Calculating the % weight deviation and comparing it to USP requirements. The tablets pass the test when no more than 2 of them differ by about twice the permitted % and no tablet does so [47].
Disintegration test: By inserting tablets in every tube of the disintegration test apparatus and positioning the basket rack assembly in a 1-liter beaker containing water at 37⁰C, simulated gastric fluid or intestinal fluid, the tablet disintegration time was measured. The basket is raised and lowered by a conventional motor over a length of 5 cm-6 cm with a frequency of 28 cpm-32 cpm. USP disintegration test would indeed be considered effective when all of the pills crumble and fragments filter across the #10 mesh sieve in the given time.
Uniformity of drug content: Using the procedure outlined in each separate monograph, the contents of 10 dosage units are individually assessed using the USP method. The concentration of each dosage unit’s active component must fall between 85% and 115% of the label claim, and the SD should be under 6%, unless otherwise specified in the monograph. Additional testing in accordance with the USP requirements is necessary if more than one dosage form units fail to these requirements [48].
In vitro dissolution studies
Utilizing USP Type I Apparatus, an in vitro dissolution investigation is carried out (Basket type). Tablet added to 900 ml of fluid that dissolves, either phosphate buffer solution with a pH of 7.4, 0.1 N HCl, or simulated stomach juice. The dissolving medium is kept at a temperature of 37⁰C ± 0.5⁰C by a stirrer spinning at a fixed rpm. 5 ml of samples collected at various times periods were substituted with new medium and assessed in a UV spectroscope to determine absorbance. This was done using the appropriate blank solution. Finally, a suitable equation is used to calculate the medication release rate [49].
Release kinetics studies
Various release kinetic models are as follows.
Zero order release model: Systems wherein the drug release rate is regardless of its quantity are described by zero order models.
C = k0t
where C is the cumulative percentage of the medication released and ko is the zero-order constant, t represents time. If the drug follows zero order kinetics, a straight line having a slope (ko) is produced when time is plotted against the cumulative percentage of drug released.
First order release model: Systems whose release rate and concentration are correlated are described by a 1st order model.
where C signify the cumulative percentage of the medication remaining, and Co indicate the drug’s initial concentration. k signify the first order constant. When first order kinetics are used, a graph of time against the logarithm of the cumulative percentage of drug left in the body results in a straight line having a slope of (k/2.303).
Higuchi release model
According to the Higuchi model, the drug release rate and drug diffusion are correlated when the solid drug is disseminated in an insoluble matrix.
Q = kt1/2
Where Q is the cumulative proportion of the medicine released and k is a constant that reflects the system’s design parameters. t represents time. If the Higuchi kinetics are followed, a straight line results from plotting the square root of time on the x-axis against the cumulative % of drug released on the y-axis.
Hixson-crowell release model
The drug release that results from a shift in the dimensions of the tablets is described by the Hixson-crowell model.
Qo-1/3- Qt 1/3 = KHC t
where Qt is the total quantity of medication released during time t, Qo is the drug’s starting dosage, and K HC is the rate constant in the Hixson-crowell rate equation. If the Hixson-Crowell kinetics are followed, a straight-line result from plotting time and the cube root of the cumulative % of medication remaining.
Korsmeyer and peppas model
Using a polymeric system equation, the Korsmeyer and Peppas model derives a linear connection that represents the drug release.
Mt/M∞ = k t n
where Mt/M∞ represents proportion of drug released at time t, k-Release rate constant n-Release exponent
If the kinetics described by Korsmeyer and Peppas are followed, a straight-line result from plotting of log time vs log cumulative % of medication released.
Scanning Electron Microscopy (SEM)
For studying the drug release pattern from the created formulations, a scanning electron microscope was employed to examine surfaces coated tablets prior to and following investigations of dissolution. Membranes were placed between wax paper sheets and dried at 45⁰C for 12 h before being examined. Using double-sided tape to secure them, the samples (membranes) were then vacuumcoated with gold with the help of a sputter coater. In a SEM equipped with an ion sputtering apparatus, scans were obtained at a 20 KV excitation voltage. Prior to and following dissolution, surface of the membrane coated with the optimum formulation film coating was investigated, and the capacity of the porogen and drug release could be assessed by contrasting the porous morphology [50].
In vitro evaluation
For calculating the rate at which a medication is delivered in vitro via an osmotic drug delivery system, there are several approaches that are viable. Osmotic pumps are contained in loosely woven bags made up of nylon or polyethylene, which are affixed onto a rod that is hooked to a horizontal transfer arm linked to a vertically reciprocating shaker. A known quantity of release medium is then placed into test tubes or other containers, over which the arms carrying various systems are subsequently placed. By employing a temperature-regulated water bath, the medium’s temperature is maintained at 37°C ± 0.5°C. The systems are then vertically agitated while being submerged in the release media and the shaker is operated. Systems are withdrawn from the first receptor container after a certain amount of time (usually 1 h-2 h) and transported (manually or mechanically) to a 2nd receptor container, where the mixing is then performed. The process is repeated until the systems have been evaluated for a predetermined amount of time-between 12 h and 24 h, based on the type of formulation. Now, using the appropriate procedure, each receptor solution is examined for the presence of drugs. The release rate may be calculated by dividing quantity of medication in each container by the test interval’s duration (in h). By summing the quantities from the various periods, the cumulative quantity released is therefore calculated. As was already mentioned, the medication releases from the ODDS with a zero-order kinetics. To determine if it produces a consistent drug release profile, the overall quantity of medicines released from the optimized formulation over various time periods are fitted to zero order kinetics with the least squares technique of analysis.
In vivo evaluation
It was found that the dog’s digestive tract’s environment, both with respect to pH and motility, and that of humans, are quite comparable. As a result, dogs are frequently employed to test the rate of medication delivery in vivo from an osmotically regulated oral drug delivery device. The GI transit of an ODDS is assessed by radio labelling a whole osmotic tablet for establishing IVIVC. Gamma scintigraphy is used to track the unit’s movement in the GI tracts of young and elderly, healthy subjects [51-56] (Table 6).
Table 6: CPOP-related patents
| S.No | U.S. Patent number | Type of osmotic system |
|---|---|---|
| 1. | US4,968,507 | Osmotic pumping with regulated porosity |
| 2. | US4,256,108 | Microporous semipermeable laminated osmotic system |
| 3. | US4,880,631 | Diltiazem L-maleate osmotic pump with controlled porosity |
| 4. | US4,160,452 | Lamellar osmotic system with semipermeable and microporous laminae |
| 5. | US4,994,273 | Delivery of drugs with weak aqueous solubility using a solubility-regulated CPOP |
| 6. | US4,946,686 | Delivery of drugs with weak aqueous solubility using a solubility-regulated CPOP |
Necessity for the development of CPODD:
• To decrease the administration dosage form
• Using this formulation one can decrease the dose related drawbacks
Improve in Patient compliance by achieving the controlled issue process.
Artificial intelligence for osmotic drug delivery system
Using AI in the pharmaceutical and delivery systems: The use of deep learning, protein function prediction, compound library creation, and the identification of new drug candidates are all important aspects of contemporary drug discovery. The use of artificial intelligence platforms in the biopharmaceutical industry for the analysis of biological data, identification of therapeutic targets, and search for various medicines may improve the efficiency of drug discovery. Early on in the drug development (Figure 11).
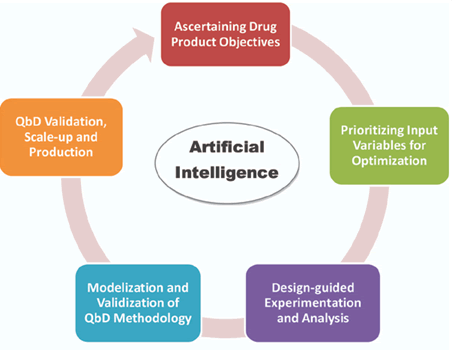
Figure 11: Artificial intelligence objectives
Implementation of nanorobots in therapeutics: The advancement of micro and nano-electromechanical systems has paved the way to the fabrication of implantable robots for a numerous applications, notably, the controlled drug/gene-delivery. Nanorobots that can operate entirely on their own power source or require the help of an external one, as well as ones that include sensors and artificial intelligence, have gained a lot of attention as a result of the astonishing developments in nanotechnology. These intelligent buildings can process data in a variety of ways.
Reasons why target fishing is very important: In the context of drug design, a clear understanding of the molecular targets may be of paramount importance. Target Fishing (TF) is a crucial part of contemporary drug discovery, since it is used to forecast the treatments’ targets, methods of action, and adverse effects. With the use of machine learning algorithms and cheminformatics toolkits, researchers may get a more in-depth understanding of the structures of intricate molecules and propose innovative therapeutic candidates to combat complex illnesses (Figure 12).
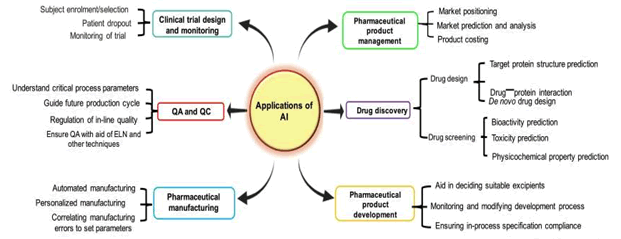
Figure 12: Application of AI in pharmaceutics
Complex problems and their possible solutions: Improvements in drug screening procedures and the designing of innovative drug delivery approaches, notably feedback-controlled, programmable, and microchipbased technologies, have been possible because of the introduction of state-of-the-art and high-performance methodologies and tremendous breakthroughs in computer science. There are still a number of vexing problems that are yet to be resolved about the capacity of the drug reservoir in implanted drug delivery devices.
Conclusion
Osmosis-induced pressure serves as the basis for how CPOD releases drugs. CDDS can help prolong the release of the drug and found to have considerable activity with the necessity of fewer doses when using this CPOD formulation designed for single drug therapy or multiple drug treatment. According to earlier data, this formulation reduces hypertension with a lower dose over a shorter period of time and is also efficacious in multi-drug regimens. High polar soluble to low polar soluble drugs can be formulated into controlled release osmotic porosity drug formulation form which helps for the delayed release of drug, this designing process is also cost effective and easy. Future research will likely focus on developing a number of different types of osmotic systems, including those that utilize pulsatile delivery that works on an expandable orifice, telescopic capsules that included tiny osmotic pumps for extended release, lipid-based osmotic pumps. This review on CPOD can help the researchers in carrying out the work using this formulation process.
Acknowledgement
None.
Conflict Of Interest
Authors have no conflict of interest to declare.
References
- Maneeshkumar, A text book of novel drug delivery system, Sia Publishers, 2020.
- Y. Yoshioka, T. Ochiya, Exosome as novel nanocarriers for therapeutic delivery, Drug Deliv Syst, 35(2020):35-46.
- R. Sareen, N. Jain, D. Kumar, An insight to osmotic drug delivery, Curr Drug Deliv, 9(2012):285-96.
- G.M. Patel, J.D. Patel, Single Core Osmotic Pump (SCOP): Development of single layer osmotic controlled release tablet for poorly soluble drug, J Pharm Technol Drug Res, 1(2012):1.
- S. Srikonda, P. Kotamraj, B. Barclay, Osmotic controlled drug delivery systems, design of controlled release drug delivery systems, McGraw Hill, (2006):203.
- B.S. Venkateswarlu, C. Pasupathi, A. Pasupathi, Osmotic drug delivery system: A review, J drug Deliv ther, 9(2019):759-64.
- B.P. Gupta, N. Thakur, N.P. Jain, Osmotically controlled drug delivery system with associated drugs, J Pharm Pharm Sci, 13(2010):571-88.
- A. Grattoni, M. Merlo, M. Ferrari, Osmotic pressure beyond concentration restrictions, J Phys Chem B, 111(2007):11770-5.
- S. Herrlich, S. Spieth, S. Messner, Osmotic micropumps for drug delivery, Adv Drug Del Rev, 64(2012):1617-27.
- T. Ghosh, A. Ghosh, Drug delivery through osmotic systems an overview, J Appl Pharmal Sci, 1(2011):38-49.
- S. Rose, J. Nelson, A continuous long-term injector, Aust J Exp Biol Med Sci, 33(1955):415-21.
- F. Theeuwes, T. Higuchi Inventors; Alza Corporation, Palo Alto, CA, Assignee. Osmotic dispensing device for releasing beneficial agent, US Patent No. 3845770, 1974.
- F. Theewes, Elementary osmotic pump, J Pharm Sci, 4(1975):1987-91.
- R. Amit, D. Prabakaran, P. Singh, Modified push pull osmotic system for simultaneous delivery of theophylline and salbutamol, Int J Pharm, 284(2004), 95-108.
- S. Padma, V. Ravichandram, V. Suba, A review on osmotic drug delivery system, Int J Res Pharm Biomed Sci, 4(2013):810-21.
- G.M. Zentner, G. S. Rork, Himmelstein osmotic flow through controlled porosity films an approach to delivery of water-soluble compounds, J Control Release, 2(1985):217-29.
- L.S. Sanap, A.D. Savkare, Controlled porosity osmotic pump a review, Inter J Pharma Res Dev, 5(2014):71-80.
- W.C. Kenneth, C.B. Maccdonald, R.C. Michael, Extrudable core system: development of single-layer osmotic controlled-release tablets, J Control Rel, 134(2008): 201-206.
- S.M. Herbig, J.R. Cardinal, R.W. Korsmeyer, K.L. Smith, Asymmetric membrane tablet coatings for osmotic drug delivery, J Control Release, 35(1995):127-36.
- B. Lindstedt, G. Ragnarsson, J. Hjartstam, Osmotic pumping as a release mechanism for membrane coated drug formulations, Int J Pharm, 56(1989):261-8.
- C.K. Sahoo, S.R.M Rao, M. Sudhakar, Advances in osmotic drug delivery system, J Chem Pharm Res, 7(2015):252-73.
- L. S. Sanap, A. D. Savkare, Controlled porosity osmotic pump a review, Inter J Pharma Res Dev, 5(2014):71-80.
- C.A. Babu, M.P. Rao, V.J. Ratna, Controlled porosity osmotic pump tablets an overview, J Pharm Res Health Care, 2(2010):114-26.
- D.R. Swanson, B.R. Barclay, P.S.L. Wong, Nifedipine gastrointestinal therapeutic system, Am J Med, 83(1987):3-9.
- A.G. Thombre, A.R. DeNoto, D.G. Gibbes, Delivery of glipizide from asymmetric membrane capsules using encapsulated excipients, J Control Release, 60(1999):333-41.
- H. Patel, U. Patel, H. Kadikar, A review on osmotic drug delivery system, Int Res J Pharm, 3(2012):89-94.
- R.L. Jerzewski, Y. Chien, Osmotic drug delivery treatise on controlled drug delivery: Fundamentals, optimization, application, Marcel Dekker; 225(1992):53.
- N.B. Khavare, S.F. Dasankoppa, N.G. Najundaswamy, A review on key parameters and components in designing of osmotic controlled oral drug delivery systems, Indian J Novel Drug Del, 2(2010):122-31.
- S. Padmapriya, V. Ravichandran, V. Suba, A review on osmotic drug delivery system, Int J Res Pharm Biomed Sci, 4(2013):810-21.
- M.S. Thorat, P.S. Anita, R. Virprasad, C.S. Meera, Overview of past and current osmotic drug delivery systems, Int J Pharm Chem Sci, 1(2012):743-53.
- M. Kelbert, S.R. Bechard, Evaluation of cellulose latex as coating material for controlled release products, Drug Dev Ind Pharm, 18(1992):519-38.
- P.H. Nikam, J.A. Kareparamban, A.P. Jadhav, A review on controlled porosity osmotic pump tablets and its evaluation, Res J Pharma Biol Chem Sci, 3(2012):478-93.
- L. Dong, P. Wong, S. Espinal, A new osmotic delivery system for controlled release of liquid formulations, in: Proceedings of the International Symposium on controlled release of biomedical materials, San Dieego, 2001.
- R.K. Verma, B. Mishra, S. Garg, Osmotically controlled oral drug delivery, Drug Dev Ind Pharm, 26(2000):695-708.
- N.B. Khavare, S.F. Dasankoppa, N.G. Najundaswamy, A review on key parameters and components in designing of osmotic controlled oral drug delivery systems, Indian J Novel Drug Del, 2(2010):122-31.
- J. Guo, An investigation into formation of plasticizer channels in plasticized polymer films, Drug Dev Ind Pharm, 20(1994):1883-93.
- L.C. Dong, S. Espinal, P.S.L. Wong, Inventors Alza Corporation Mountain View CA Assignee. Dosage form comprising liquid formulation, US Patent, 6174547(2001).
- M. Manikandan, K. Kannan, R. Manavalan, Compatibility studies of camptothecin with various pharmaceutical excipients used in the development of nanoparticle formulation, Int J Pharm Pharm Sci, 5(2013):315-21.
- M.M. Jadav, S.R. Teraiya, K.N. Patel, Formulation and evaluation of oral controlled porosity pump tablet of zaltoprofen, Int J Pharma Res Sci, 1(2012):254-67.
- A. De Ryck, R. Condotta, J.A. Dodds, Shape of cohesive granular heap, Powder Technol, 157(2005):72.
- S. Verma, S. Saini, A. Rawat, Formulation, evaluation and optimization of osmotically controlled colon targeted drug delivery system, J Pharm Sci Res, 3(2011):1472-85.
- H. Patel, U.D. Patel, H. Kadikar, Formulation and evaluation of controlled porosity osmotic pump tablets of glimepiride, Int J Drug Del, 4(2012):113-24.
- M. Ali, K. Senthil, S. Parthiban, Formulation and evaluation of controlled porosity osmotic tablets of prednisolone, Int J Pharm, 3(2013):70-8.
- S. Edavalath, K. Shivanand, K. Prakasam, Formulation development and optimization of controlled porosity osmotic pump tablets of diclofenac sodium, Int J Pharm Sci, 3(2011), 438-46.
- R.M. Chandira, P. Palanisamy, B. Jayakar, Formulation and in vitro evaluation of sustained release tablet of isosorbide-5-mononitrate by porous osmotic technology, Int J Pharm Ind Res, 2(2012):400-15.
- M. Kulshrestha, R. Kulshrestha, Formulation and evaluation of osmotic pump tablet of cefadroxil, Int J Pharm Pharm Sci, 5(2013):114-8.
- Z.A. Khan, R. Tripathi, B. Mishra, Design and evaluation of Enteric Coated Microporous Osmotic Pump Tablet (ECMOPT) of quetiapinefumarate for the treatment of psychosis, Acta Pol Pharm Drug Res, 69(2012):1125-36.
- The USP 26-National Formulary 21 Rockville MD US pharmacopoeial convention, 2003.
- S. Padmapriya, V. Ravichandran, V. Suba, Development and evaluation of swellable elementary osmotic pump tablets of metoprolol succinate and ramipril, Glob J Pharmacol, 7(2013):179-86.
- R. Kumaravelrajan, N. Narayanan, V. Suba, Development and evaluation of controlled porosity osmotic pump for nifedipine and metoprolol combination, Lipids Health Dis, 10(2011):51.
- G.M. Zentner, G.S. Rork, K.J. Himmnelstein, Controlled porosity osmotic pump, US Patent No.4968507, 1990.
[Crossref] [Google Scholar]
- F. Theeuwes, L. Altos, Microporous semipermeable laminated osmotic system, US Patent No.4256108, 1981.
- J.L. Haslam, G.S. Rock, Controlled porosity osmotic pump, US Patent No. 4880631, 1989.
- F. Theeuwes, L. Altos, Calif, Osmotic system having laminated wall comprising semipermeable lamina and microporous lamina US patent No. 4,160,452, 1979.
- G.M. Zentner, G.A. McClelland, Solubility modulated drug delivery device, US patent, 4994273, 1991.
- G.A. McClelland, G.M. Zentner, Solubility modulated drug delivery system, US patent, 4946686, 1990.
Copyright: ©2023 Ismail Y, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.